Abstract
Background. In the last decade major advances have been made in the management of AL amyloidosis, such as the use of free light chains (FLC) and cardiac biomarkers in diagnosis, risk assessment, and evaluation of response, and the introduction of novel agents in the therapeutic armamentarium. However, available studies on the natural history of this disease are based on data collected before this era, and large comparative studies on novel agents are still lacking. We report the outcome of the 984 consecutive patients diagnosed between 2004 and 2014 at the Pavia Amyloidosis Research and Treatment Center (ARCT).
Methods. Baseline evaluation and therapeutic strategy were protocolized. Patients were prospectively followed for response and survival. Response was assessed by intent to treat.
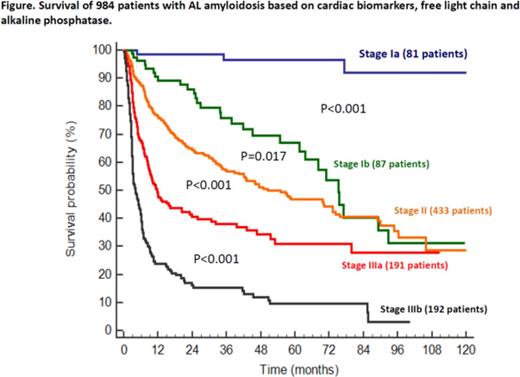
Results. Overall, the heart was involved in 76% (Mayo stage III 39%), the kidney in 66% (stage III 15%), the liver in 14%, the soft tissues in 17%, and the peripheral nervous system (PNS) in 12%. Isolated involvement of the heart or kidney was observed in 17% and 14% of cases, respectively, while the liver or PNS were the only organs involved in <1% of patients. Most common upfront treatments were melphalan-dexamethasone [MDex, 354 patients, overall hematologic response (HR) 51%, very good partial or complete response (VGPR/CR) 37%], cyclophosphamide-bortezomib-dexamethasone (CyBorD, 295 patients, HR 53%, VGPR/PR 39%), and bortezomib-MDex [BMDex, 128 patients, HR 64% (P=0.010 compared to MDex; P=0.033 compared to CyBorD), VGPR/PR 52% (P=0.002 compared to MDex; P=0.0011 compared to CyBorD)]. Amongst responders, exposure to bortezomib upfront was associated with a longer time to second-line treatment (median 43 months vs. not reached, P=0.004). After a 36-month median follow-up of living patients, overall median survival was 40 months. Mayo stage predicted survival, with 86%, 57%, and 27% of stage I, II, and III patients surviving 3 years, respectively (P<0.001). Stage III patients could be divided into 2 groups based on whether NT-proBNP was below (stage IIIa) or above (stage IIIb) 8500 ng/L (3 year survival 38% vs. 15%, P<0.001). Fifty-nine percent of stage IIIb patients died in the first 6 months, and 76% within 1 year from diagnosis. Mayo stage I could also be divided into 2 groups, with stage Ia patients having both normal alkaline phosphatase and dFLC <100 mg/L (3 year survival 97% vs. 76%, P<0.001). The only 3 deaths in stage Ia patients were not disease-related, while liver and heart failure were responsible of most deaths in stage Ib. We propose a novel 5-stage system for prognostication of survival (Figure). In the overall population, the outcome was not different in patients treated upfront with MDex, CyBorD, and BMDex (48%, 55%, and 55% at 3 years, respectively, P=0.720). However, exposure to bortezomib upfront was associated with longer survival in stage Ib patients (95% vs. 73% surviving 3 years, P=0.044), while there was no significant advantage of BMDex or CyBorD over MDex in the other stages. A high FLC burden (dFLC >180 mg/L) was associated with poorer survival in stage II patients treated with MDex (38% vs. 68% at 3 years, P<0.001) and CyBorD (50% vs. 70% at 3 years, P=0.033), but not in subjects treated with BMDex (67% vs. 70% at 3 years, P=0.401).
Conclusion. The outcome of patients with AL amyloidosis is extremely heterogeneous, but can be accurately predicted based on biomarkers of organ damage and FLC concentration. The extensive use of upfront bortezomib prolongs the duration of response, but does not translate in a general improvement of survival. This might be due to the fact that most patients refractory to or relapsed after MDex were rescued with bortezomib. However, accurate stratification reveals subgroups of patients in whom bortezomib combinations are most effective. In stage Ib patients bortezomib triplets grant the best outcome, while the combination of bortezomib, melphalan, and dexamethasone should be preferred in subjects with moderate cardiac dysfunction and elevated FLC burden.
Off Label Use: Bortezomib in AL amyloidosis. Merlini:Millennium Takeda: Honoraria; Janssen Cilag: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal