Abstract
Introduction
The difference in origin between nodal and extranodal DLBCL may contribute to the distinct clinical outcomes and prognoses. Previous studies including patients with both limited and advanced diseases showed various clinical results. The purpose is to study the clinical characteristics, and outcomes of patients with limited stage DLBCL according to the primary site of lymphoma.
Methods
From the 4,371 patients in a multi-institutional registry of newly diagnosed lymphoma in Thailand between 2007-2014, there were 920 patients with limited stage DLBCL, excluding those with primary central nervous system lymphoma. The baseline patient characteristics and clinical outcomes were analyzed according to the primary site of diseases.
Results
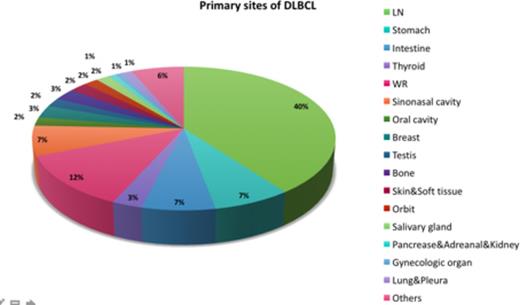
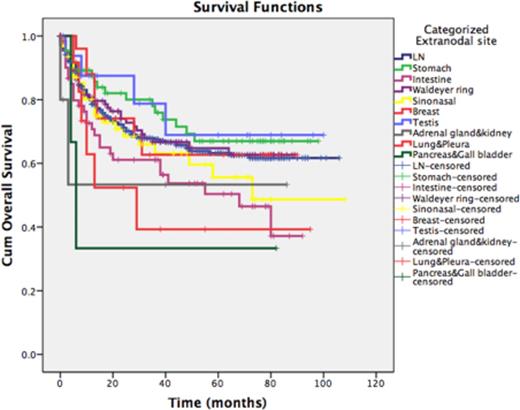
Majority of patients had extranodal diseases (n= 535, 58.2%) while the other 385 cases (41.8%) had nodal DLBCL. The five most common primary sites of extranodal disease were Waldeyer ring (12.2%), stomach (7.3%), intestine (6.8%), sinonasal cavity (6.7%) and breast (2.8%) (Figure 1). Baseline characteristics, treatment and responses were well balanced between the two groups except for a slightly higher proportion of stage I disease in extranodal DLBCL (36.8% vs 28.8%, P =0.01) (Table 1). Two-third of patients received CHOP chemotherapy while the others were treated with R-CHOP. Radiotherapy (RT) was delivered to one-fifth of the patients in each group. Overall response rates were comparable between patients with nodal and extranodal diseases (68.6% vs 66.7%). With a median follow up of 52 months, there were no significant differences of progression free (PFS) (57.6 vs. 60.8%, P =0.46) and overall survival (OS) (63.1% vs. 65.6%, P =0.20) between patients with extranodal and nodal diseases. Among patients with extranodal manifestations, those with primary lymphoma at pancreas & gall bladder, pleura & lung, adrenal gland & kidney and intestine had the worst 4-year OS (33.3%, 39.3%, 53.3%, and 53.7%, respectively) (Figure 2). RT improved PFS (71.7% vs. 54.5%, P =0.03) and OS (74.7% vs. 62.9%, P =0.02) only in primary nodal DLBCL. The two prognostic factors for survivals were being treated with R-CHOP (HR for PFS 0.84, 95%CI: 0.74-0.96; HR for OS 0.70, 95%CI: 0.55-0.91) and the IPI scores (HR for PFS 1.49, 95%CI: 1.24-1.80; HR for OS 1.86, 95%CI: 1.37-2.51).
Conclusion
Among limited stage DLBCL in Thailand, primary extranodal disease was more common than the nodal manifestations. Primary sites of origins did not affect baseline characteristics as well as the outcomes. Patients with unusual site lymphomas, however, had an inferior survivals warranted a further investigational therapy.
The clinical characteristics of limited stage DLBCL according to disease of origin
| Clinical characteristics . | Nodal DLBCL (n = 385) . | Extranodal DLBCL (n = 535) . | p-value . |
|---|---|---|---|
| Male | 205 (53.2%) | 294 (55%) | 0.60 |
| Median age (years) | 54.9 | 56.2 | 0.23 |
| Stage Stage I Stage II | 111 (28.8%) 274 (71.2%) | 197 (36.8%) 338 (63.2%) | 0.01 |
| HIV seropositivity | 11 (3.4%) | 19 (4.3%) | 0.53 |
| Age ≥ 60 | 164 (42.6%) | 230 (43%) | 0.90 |
| High serum LDH | 183 (47.5%) | 230 (43%) | 0.17 |
| ECOG ≥ 2 | 46 (11.9%) | 60 (11.2%) | 0.73 |
| IPI Low (IPI = 0-1) Low-intermediate (IPI =2) High-intermediate (IPI = 3) | 285 (74.0%) 81 (21.0%) 19 (4.9%) | 406 (75.9%) 108 (20.2%) 21 (3.9%) | 0.82 |
| Chemotherapy regimens R-CHOP CHOP | 98 (29.0%) 227 (67.2%) | 160 (33.7%) 286 (60.2%) | 0.25 |
| Radiotherapy | 94 (24.9%) | 120 (22.8%) | 0.46 |
| Response Overall response Complete response | 261 (68.6%) 227 (59.7%) | 352 (66.7%) 322 (61%) | 0.24 |
| Clinical characteristics . | Nodal DLBCL (n = 385) . | Extranodal DLBCL (n = 535) . | p-value . |
|---|---|---|---|
| Male | 205 (53.2%) | 294 (55%) | 0.60 |
| Median age (years) | 54.9 | 56.2 | 0.23 |
| Stage Stage I Stage II | 111 (28.8%) 274 (71.2%) | 197 (36.8%) 338 (63.2%) | 0.01 |
| HIV seropositivity | 11 (3.4%) | 19 (4.3%) | 0.53 |
| Age ≥ 60 | 164 (42.6%) | 230 (43%) | 0.90 |
| High serum LDH | 183 (47.5%) | 230 (43%) | 0.17 |
| ECOG ≥ 2 | 46 (11.9%) | 60 (11.2%) | 0.73 |
| IPI Low (IPI = 0-1) Low-intermediate (IPI =2) High-intermediate (IPI = 3) | 285 (74.0%) 81 (21.0%) 19 (4.9%) | 406 (75.9%) 108 (20.2%) 21 (3.9%) | 0.82 |
| Chemotherapy regimens R-CHOP CHOP | 98 (29.0%) 227 (67.2%) | 160 (33.7%) 286 (60.2%) | 0.25 |
| Radiotherapy | 94 (24.9%) | 120 (22.8%) | 0.46 |
| Response Overall response Complete response | 261 (68.6%) 227 (59.7%) | 352 (66.7%) 322 (61%) | 0.24 |
*IPI: International prognostic index
Overall survival of patients with limited stage DLBCL according to primary sites of lymphoma
Overall survival of patients with limited stage DLBCL according to primary sites of lymphoma
Khuhapinant:Roche: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal