Abstract

Background: In primary myelofibrosis (PMF), ̴ 88% of patients harbor JAK2, CALR or MPL, with respective mutational frequencies of approximately 60%, 22% and 6%; ̴ 12% are wild type for all three driver mutations and are labelled as being "triple negative" (Blood. 2014;124:2507). It is now well-established that CALR-mutated patients with PMF display significantly better survival, compared to all the other mutational categories; in addition, preliminary data have suggested inferior survival for "triple-negative" cases (Leukemia. 2014;28:1472; Blood. 2014;124:1062) and the possibility that the favorable impact of CALR mutations might be restricted to CALR type 1 or type 1-like variants (Blood. 2014;124:2465). In the current study, we sought to clarify the prognostic impact of driver mutations, and CALR variants, on overall (OS) and leukemia-free (LFS) survival, in a two-center study involving 1118 patients.
Methods: A total of 1118 patients with PMF from the Mayo Clinic (n =722) and University of Florence, Italy (n =396) were included in the current study. Study patients were selected based on availability of mutation information. PMF diagnosis was according to World Health Organization criteria (Blood. 2009;114:937). Previously published methods were used for CALR, JAK2 and MPL mutation analyses and determination of CALR variants (Blood. 2014;124:2465). Kaplan-Meier survival analysis was considered from the date of first referral for the Mayo cohort and date of diagnosis for the Florence cohort. Leukemic transformation events replaced death as the uncensored variable during LFS analysis and Cox proportional hazard regression model was used for multivariable analysis.
Results:
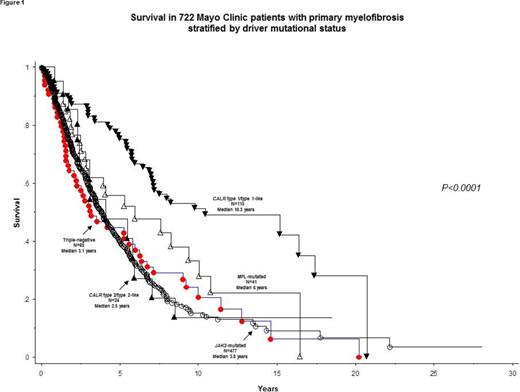
Analysis was first conducted on the Mayo cohort of 722 patients (median age 64 years; 64% males). DIPSS-plus risk distributions were 14% low, 17% intermediate-1, 37% intermediate-2 and 33% high. All patients were annotated for JAK2/CALR/MPL mutations as well as CALR variants; 477 harbored JAK2, 139 CALR and 41 MPL mutations; 65 patients were triple-negative. The 139 CALR -mutated patients included type 1/type 1-like (n =115) and type 2/type 2-like (n =24).
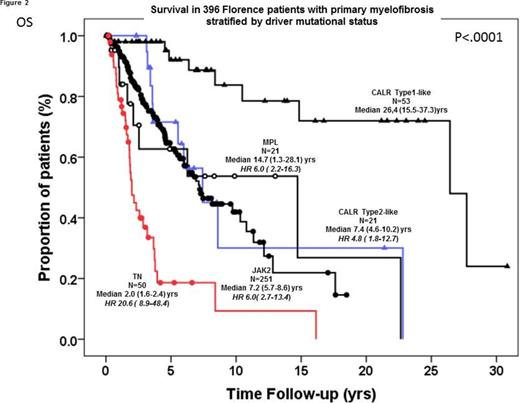
At a median follow-up time of 3.1 years, 439 (61%) deaths and 63 (8.7%) blast transformations were documented. In univariate analysis, survival in patients with CALR type 1/type 1-like mutations was significantly longer than every other mutational category: HR (95% CI) were for triple-negative 2.7 (1.8-4.0), JAK2 2.7 (2.0-3.7), CALR type 2/type 2-like 2.3 (1.3-4.2) and MPL 1.9 (1.1-3.1) (Figure 1); these differences were sustained during multivariable analysis that included ASXL1 mutations (n =480) and DIPSS-plus, and were also apparent in the Florence cohort of 396 cases that included 251 JAK2, 53 CALR type 1/type 1-like, 21 CALR type 2/type 2-like, 50 triple-negative and 21 MPL mutated cases (Figure 2). There was no difference in survival among the Mayo cohort across mutational categories not including CALR type 1/type 1-like variants (p=0.33). Because specific driver mutations in PMF differentially cluster with age and sex, multivariable analysis including these two parameters was also performed and confirmed the significant survival advantage of CALR type 1/type 1-like over triple-negative, JAK2 and CALR type 2/type 2-like mutated cases.
Based on the above information, we divided driver mutational categories into "type 1/type 1-like" (median survival 10.3 years) and "all other mutational categories" (median survival 3.9 years; p<0.01). The difference in survival between these two groups remained significant (HR 2.1, 95% CI 1.5-2.9) during multivariable analysis that included both DIPSS-plus (P<0.01) and ASXL1 mutation (HR 1.8, 95% CI 1.4-2.2). LFS was similar between these two groups (p=0.4) but it was inferior in triple-negative cases compared to CALR type 1/type 1-like variants (HR 2.8, 95% CI 1.3-6.2), MPL (HR 4.6; 95% CI 1.04-20.4) and JAK2 (HR 2.5, 95% CI 1.3-4.8) but not CALR type 2/type 2-like variants (p=0.56). There was no difference in LFS among mutational categories not including triple-negative cases (p=0.33).
Conclusions: In PMF, driver mutations might be classified into two prognostically distinct categories: "favorable" (type 1/type 1-like) and "unfavorable" (all other mutational categories). In addition, triple-negative cases might be at a higher risk of leukemic transformation.
Pardanani:Stemline: Research Funding. Vannucchi:Novartis: Other: Research Funding paid to institution (University of Florence), Research Funding; Shire: Speakers Bureau; Baxalta: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal