Abstract
Background: Polycythemia vera (PV) is a myeloproliferative neoplasm characterized by erythrocytosis and debilitating symptoms. Patients (pts) often have elevated white blood cell (WBC) and platelet (PLT) counts. Ruxolitinib is a JAK1/JAK2 inhibitor that proved superior to best available therapy (BAT) in controlling hematocrit (HCT) and improving splenomegaly and symptoms in pts with PV who have an inadequate response to or unacceptable side effects from hydroxyurea (HU). In the phase 3 RESPONSE study, HCT control was achieved by wk 32 in 60% of pts in the ruxolitinib arm and 20% of pts in the BAT arm; 40% of pts in the ruxolitinib arm achieved ≥ 35% reductions in spleen volume from baseline at wk 32 (spleen response) vs 1% in the BAT arm. Although not all pts randomized to ruxolitinib achieved protocol-defined HCT control or a spleen response at the time of the primary analysis, 85% remained on treatment, suggesting that most pts were deriving a therapeutic benefit from ruxolitinib therapy beyond HCT and spleen responses. This was supported by a higher proportion of HCT non-responders (ie, pts who did not achieve protocol-defined HCT control) achieving a symptom response (≥ 50% reduction in MPN-SAF total score) at wk 32 compared with all pts in the BAT arm (38% vs 4%; Verstovsek et al, ASH 2014). Additionally, HCT non-responders in the ruxolitinib arm had a greater median duration of time to subsequent phlebotomy (PBT) eligibility (52 wk) compared with HCT non-responders in the BAT arm (21 wk; Verstovsek et al, ASH 2014). Here, we explore whether pts randomized to ruxolitinib who did not achieve HCT control or a spleen volume response at the time of the primary analysis were able to subsequently achieve a response with continued ruxolitinib treatment.
Methods: Pts with PV who were HU-resistant/intolerant by modified European LeukemiaNet criteria and required PBT for HCT control were randomized 1:1 to ruxolitinib 10 mg twice daily or BAT. The primary composite endpoint was the proportion of pts who achieved HCT control from wk 8 to 32 (with ≤ 1 PBT from wk 0 to 8) and a ≥ 35% reduction in spleen volume from baseline at wk 32 by MRI. HCT control was defined as a lack of PBT eligibility (HCT > 45% that was also ≥ 3 percentage points higher than baseline or > 48%, whichever was lower). The primary analysis occurred when all pts reached wk 48 or discontinued. Here, efficacy was evaluated in HCT non-responders and pts who did not achieve a spleen response at wk 32. Subsequent HCT control was defined as remaining PBT ineligible for 32 wk after the last PBT eligibility. Subsequent spleen response was defined as achieving a ≥ 35% reduction in spleen volume from baseline by MRI after wk 32.
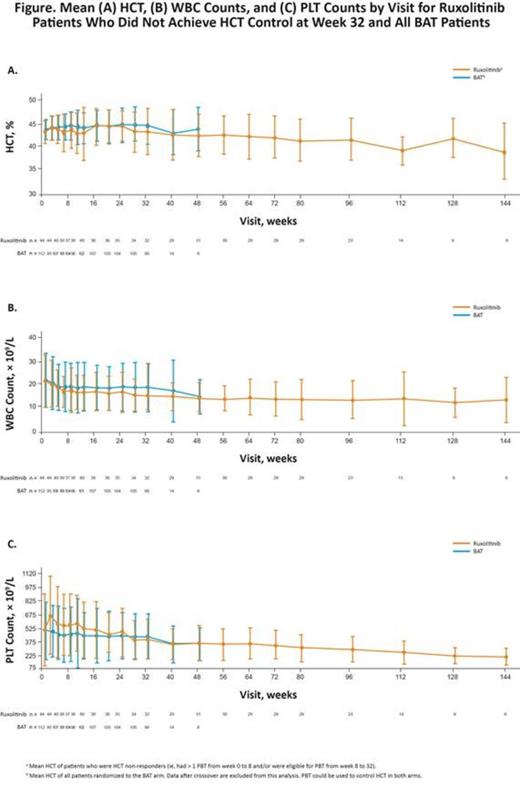
Results: Overall, 110 pts were randomized to ruxolitinib and 112 to BAT. At the 80-wk follow-up, most pts randomized to ruxolitinib remained on treatment (83%). No pts randomized to BAT remained on BAT; 88% of pts crossed over to receive ruxolitinib. Of the 44 ruxolitinib-randomized pts who did not achieve HCT control at wk 32, 31 were still receiving treatment. Of the 31 HCT non-responders remaining on treatment, 22 (71%) achieved HCT control after wk 32; 25.8%, 29.0%, and 12.9% of pts achieved HCT control at wk 48, 56, and 64, respectively. HCT non-responders experienced long-term HCT control, with mean HCT values remaining < 45%, and below those achieved in pts on BAT at all subsequent time points (Figure). A sustained improvement in WBC and PLT counts was also seen in these pts over the study period. After wk 32, mean WBC and PLT counts were consistently < 12 × 109/L and < 400 × 109/L, respectively. Similarly, of the 66 pts in the ruxolitinib arm who did not achieve a spleen response at wk 32, 54 remained on treatment; by wk 144, 24 of these pts (44.4%) had a spleen response, including 13 (24.1%) who achieved the response by wk 64.
Conclusions: In the RESPONSE study, ruxolitinib provided clinical benefits in most pts with PV who are HU-resistant/intolerant. The majority of pts who did not achieve HCT control at the time of the primary analysis subsequently did so with continued ruxolitinib treatment. In addition, many pts also experienced a subsequent spleen response and had sustained control of WBC and PLT counts, 2 clinically important hematologic parameters in PV. These findings suggest that continued ruxolitinib treatment provides therapeutic benefits over time in pts with PV, both for pts who achieve early disease control and for those who achieve subsequent responses.
Kiladjian:Novartis: Consultancy; Novartis: Other: Travel grant; Research Funding paid to institution (Hôpital Saint-Louis et Université Paris Diderot); Incyte Corporation: Consultancy. Masszi:Bristol-Myers Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis Pharmaceuticals Corporation: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen Cilag: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Jones:Incyte Corporation: Employment. Gadbaw:Novartis Pharmaceuticals Corporation: Employment, Equity Ownership. Li:Novartis Pharmaceuticals Corporation: Employment. Habr:Novarits Pharmaceuticals Corporation: Employment. Vannucchi:Shire: Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Baxalta: Membership on an entity's Board of Directors or advisory committees; Novartis: Other: Research Funding paid to institution (University of Florence), Research Funding. Verstovsek:Incyte Corporation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal