Abstract
Introduction: WHO classification of MDS is based on cytopenias, dysplasia, percentage of blasts in PB and BM, and cytogenetics. IPSS-R establishes BM blast subgroups (≤2%,2-<5%,5%-10% and >10%) with independent impact in OS. Erythroid hyperplasia (≥50% of total BM cells) is common in MDS. Concerning MDS with expanded erythropoiesis, there is no consensus whether the proportion of BM blasts should be considered on the basis of all nucleated cells (approach-A) or in non-erythroid cells (approach-B).
Aim: To elucidate this issue, we reassess percentage of BM blasts of MDS with erythropoiesis ≥50% from the Spanish registry (RESMD), according to both definitions.
Methods: We performed a retrospective analysis of 507 primary MDS diagnosed according to WHO 2008. Proportion of red-cells was calculated in 500 nucleated cells. Erythroid hyperplasia was documented in 10.4% of patients from RESMD.
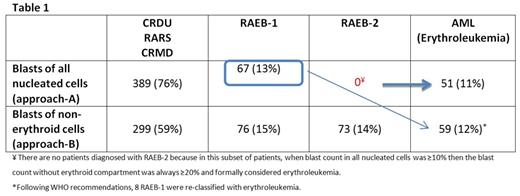
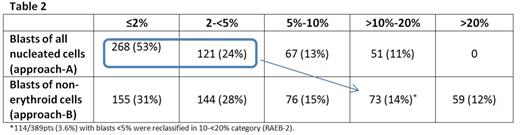
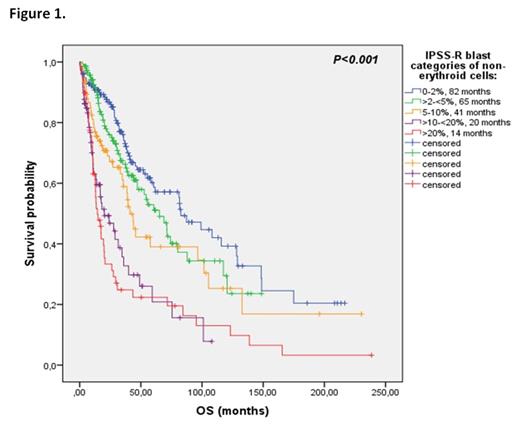
Results: Median age of presentation was 74years (25-94years) and 63% were males. Median follow-up was 29.4 months and median OS was 47.14 months. Table 1 shows distribution of WHO subtypes of the series according to both approaches. Of note, following WHO recommendations, RAEB-2 diagnosis was not possible; formally all of them were diagnosed with erythroleukemia. Distribution of patients according to IPSS-R blast-categories by both methods is shown in Table 2. It is noteworthy that 14/389pts (3.6%) with blasts <5% using approach-A were reclassified in 10-<20% category (RAEB-2) when the approach-B was applied. However, their survival did not differ significantly from those who remained in low-count blast categories. Using approach-A, IPSS-R blast categories discriminate significantly OS of blast subgroups <5% (0-2% vs. 2-<5%, 81 vs. 44 months, p =0.011). Nevertheless, categories with ≥5% blasts showed no differences (5-10% vs. 10-20%; 18 vs. 13 months, p =0.39). With approach-B, significant differences were observed among categories with <10% blasts (0-2% vs. 2-<5% vs. 5-10%; 82 vs. 65 vs. 41 months, p =0.032). However, as in IPSS-R, no differences were observed >10% (10-20% vs. >20%; 20 vs. 14 months, p =0.53). Figure 1. Applying approach-A, significant differences in proportion of patients with high-risk karyotype defined by IPSS were seen between ≥5% blasts vs. <5%, but not between 5-<10% and 10-20%. Using approach-B, these differences appeared in 10% cut-off, without differences between 10-<20% and >20%. Therefore, high-risk patients (>10% blasts and high-risk cytogenetics) were better defined by the second method.
Conclusion: In agreement with WHO committee recommendations, these results suggest that there is no a uniform criteria for assessment of medullary blasts. Considering percentage of blasts on the basis of non-erythroid compartment might improve the classification and prognostication of MDS with ≥5% blast cells. However in low-blast count patients this approach could overestimate their risk.
Valcárcel:Celgene Corporation: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; GlaxoSmithKline: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Ramos:GlaxoSmithKline: Honoraria; Janssen-Cilag: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria; Celgene Corporation: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Amgen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal