Abstract
Introduction: Allogeneic stem cell transplantation (SCT) is the only curative therapy currently available for patients with thalassemia major (TM). In developing countries, the significant delay that often occurs between diagnosis and SCT for a variety of reasons and the inadequate transfusion-chelation that most patients can access, leads to greater liver damage and advanced risk status for SCT in most of these patients. This study was therefore aimed at evaluating the outcome of SCT among a large cohort of these patients in India.
Methodology: Data on the clinical profile and outcome after allogeneic SCT carried out for patients with TM was collected from the participating centers. All patients transplanted between January 2000 and June 2014 with matched related (MRD) or unrelated donors (MUD) were included in the analysis. Conditioning regimen was based on Bu/Cy (busulfan and cyclophosphamide, ± ATG) or Treo/Thio/Flu (treosulfan, thiotepa and fludarabine) in the vast majority of patients. Graft versus host disease (GVHD) prophylaxis consisted predominantly of cyclosporine and short course methotrexate. Data was collected from prospectively maintained standardized institutional individual medical records and analyzed with the SPSS software version 16.0
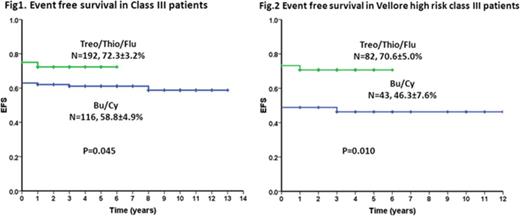
Results: Five hundred and ninety six patients [356 males and 240 females] with a median age of 7 years (range: 1 - 25) underwent allogeneic SCT during the study period. There were 560 (94.0%) children aged ≤ 15 years, while 36 (6.0%) were aged >15 years at the time of SCT. Majority of the patients belonged to Pesaro class 3 (n=310; 52.0%), while 219 to class 2 (36.7%) and 67 to class 1 (11.2%). Among the 226/310 patients in Class 3, 126 (55.8%) belonged to the Vellore high risk category (age >7 years and liver size >5cms). Conditioning regimen was based on Bu/Cy (±ATG) in 315 patients (52.9%) while in 278 (46.6%) patients it was based on Treo/Thio/Flu. There was a MRD for 564 patients (94.6%) while 32 (5.4%) received the graft from MUDs. Of the total of 596 patients, 568 (95.3%) engrafted by day +28. 22 patients (3.6%) had early mortality by day +15, 23 (3.9%) more by day +28, and another 50 (8.4%) by day +100. Graft rejection was noted in a total of 38 patients (6.4%), 6 of whom were before day +28. The overall incidence of acute GVHD was 195/568 (34.3%) with grade II-IV in 25.2% (n=143) and grade III-IV was seen in 9.2% (n=52). Chronic GVHD, which was limited in most patients, was seen in 91/501 patients (18.2%) of evaluable patients. At a mean follow up of 11 years (range: 0 -14 years), the overall survival (OS) and event free survival (EFS) for the entire group are 78.9%±1.9% and 72.8%±2.1%. A total of 119 (19.9%) of patients expired - 58 (48.7%) of whom were due to infections while regimen related toxicity lead to death in 23 (19.3%), GVHD in 10 (8.4%) and 28 (23.5%) died due to other causes. The OS and EFS for the different risk categories were the following: class 1 (95.5%±2.5%, 92.5%±3.2%), class 2 (82.0%±2.6%, 75.9%±2.9%) and class 3 (72.5%±3.6%, 65.6%±3.6%), (p=0.001 and p=0.000, respectively). The OS and EFS among those with grade II to IV GVHD was 76.1%±3.6 and 75.4±3.6% while among those with grade III/IV GVHD was 40.4%±6.8, respectively. We compared the outcome in patients who received Bu/Cy based conditioning (n=315; 52.9%) with those receiving Treo/Thio/Flu based conditioning (n=278; 46.6%). In terms of their baseline characteristics, there were greater number of older and class 3 patients in the latter group. (Table 1) While the OS was comparable in the two groups, the EFS was higher among those receiving Treo/Thio/Flu with Class 3 disease (72.3±3.2% vs 58.8±4.9%; p=0.045). (Fig.1) This result was more pronounced among those with Vellore high risk class 3 disease (70.6%±5.0% vs 46.3±7.6%; p=0.010). (Fig.2)
Conclusion: The majority of patients with thalassemia major undergoing SCT in India are in the higher risk categories. The overall outcome of SCT among these patients is comparable with those reported in the literature. Treosulfan based conditioning regimen has improved outcome significantly among the high risk patients.
| . | Bu/Cy (n=315) N (%) . | Treo/Thio/Flu (n=278) N (%) . | P value . |
|---|---|---|---|
| Age <=15 >15 | 309 (98.1) 6 (1.9) | 248 (89.2) 30 (10.8) | 0.000 |
| Risk group Class 1 Class 2 Class 3 | 35 (11.1) 164 (52.1) 116 (36.8) | 32 (11.5) 54 (19.4) 192 (69.1) | 0.000 |
| Class 3 HR Class 3 LR | 43 (57.3) 32 (42.7) | 82 (54.7) 68 (45.3) | 0.776 |
| . | Bu/Cy (n=315) N (%) . | Treo/Thio/Flu (n=278) N (%) . | P value . |
|---|---|---|---|
| Age <=15 >15 | 309 (98.1) 6 (1.9) | 248 (89.2) 30 (10.8) | 0.000 |
| Risk group Class 1 Class 2 Class 3 | 35 (11.1) 164 (52.1) 116 (36.8) | 32 (11.5) 54 (19.4) 192 (69.1) | 0.000 |
| Class 3 HR Class 3 LR | 43 (57.3) 32 (42.7) | 82 (54.7) 68 (45.3) | 0.776 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal