Abstract
Background: Hematologic malignancies have been associated with poor performance on standard measures of quality of end-of-life (EOL) care in oncology (eg, Hui, Cancer, 2014); however, these measures were originally developed primarily for solid tumors, and they may not appropriately address EOL quality issues for patients with blood cancers. We sought to explore hematologic oncologists' perspectives regarding the acceptability of current oncology EOL quality measures, hypothesizing that they would report them to be largely unacceptable.
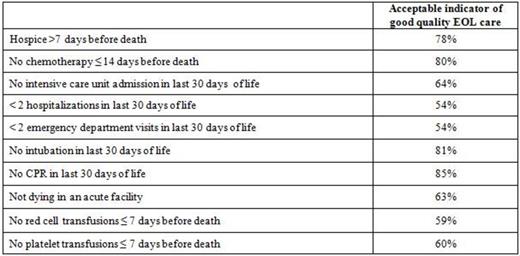
Methods: In 2014, we mailed a 30-item survey to a national sample of hematologic oncologists randomly selected from the American Society of Hematology clinical directory. The survey was developed through focus groups (n=20) and cognitive debriefing (n=5) with hematologists whose practices focus on patients with blood cancers. In the resulting survey, we provided a list of standard EOL quality measures (Earle, JCO, 2003; Keating, Cancer, 2010; Phelps, JAMA, 2009; see table) and two novel hematology-based measures (no red cell transfusions ≤ 7 days before death, and no platelet transfusions ≤ 7 days before death) and asked "Please indicate whether or not you feel each is an acceptable indicator of good quality EOL care for patients with hematologic malignancies." We decided a priori that we would consider a measure to be "highly acceptable" if there were at least 75% agreement among hematologic oncologists on its acceptability. Worrying that they might reject them all, we also asked them to identify three measures they would choose in a scenario where three had to be adopted.
Results: We received 349 surveys from 48 states (response rate: 57.3%). Non-responders were not significantly different across known variables (gender and region of practice). Among respondents, median age was 52 years, median time in practice was 25 years, and 43% practiced primarily in tertiary centers. Eighty-seven percent were board-certified in oncology, 81% in hematology, and 71% in both specialties. The table below shows acceptability of the quality measures as rated by respondents.
In the exercise where three measures had to be chosen, the one chosen most often was no CPR within 30 days of death (54%), followed by enrollment in hospice >7 days before death (46%).
Conclusions: In contrast to our hypothesis, all of the measures we presented were considered acceptable by a substantial proportion of the hematologic oncologists in our national cohort. Moreover, while four of the measures reached our a priori designation of being highly acceptable, the two hematology-focused measures did not meet this same threshold. These data suggest that in hematologic oncology, resources should be directed towards addressing barriers to performance on established EOL quality measures in addition to creating new ones.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal