Abstract
Introduction
Portal and/or splenic vein thrombosis (PVST), stemming from immune thrombocytopenia (ITP), warm autoimmune hemolytic anemia (wAIHA) or other splenic diseases, is highly associated with splenectomy complications. Although symptomatic PVST is a rare event (incidence rate 1-3%) reportedly associated to mortality, it has been shown through systematic computed tomography (CT) scans that PSVT events exist in up to 50% of splenectomized patients. The clinical significance of this finding remains unclear. Indications of anticoagulation depend on the site and extent of PSVT. The relevance of postoperative CT scanning is discussed, specifically in the context of immune cytopenia, where PSVT seems to be less frequent and less extended. We conducted a retrospective study to assess the incidence, the sites and the outcome of PSVT in ITP and wAIHA patients.
Patients and methods
The study was conducted between 2009 and April 2015 in a tertiary-care center for immune cytopenias (Henri Mondor Hospital, France) where postoperative CT scans are systematically performed. We analyzed splenectomized ITP or wAIHA (without underlying malignancy) adult patients undergoing a postoperative enhanced abdominal CT scan. Clinical and biological data were collected from medical records. All CT scans were reviewed by a senior radiologist using a standardized form.
Results
Thirty nine patients (19 men, 20 women), with a mean age of 45 years (range, 19-83), were splenectomized mostly by laparoscopic surgery (n=38), for ITP (n=30) or wAIHA (n=9). Thirty six patients (92%) had received a preventive anticoagulation treatment for a median duration of 24 post-operative days (range, 7-36). Among ITP patients, the mean preoperative platelet count was 95.6 G/L (SD: 97). ITP patients had received corticosteroids (75%), intravenous immunoglobins (43%), or thrombopoietin receptor agonists (41%) in preparation for splenectomy). The overall initial response rate at 2 months from splenectomy was 69% (ITP: 63%, wAIHA: 89 %).
The CT scan was performed within 5 days on average (range: 3-12) of splenectomy. The incidence rate of PSVT was 74% (29/39), without discrimination between ITP (22/30, 73%) and wAIHA (7/9, 78%, p = 0.79) (Table 1). There were mostly distal splenic vein (dSVT) (n=14), or dSVT associated with intrahepatic portal vein thrombosis (iPVT) (n=12). There were no mesenteric vein thromboses, 1 extrahepatic portal vein (ePVT) and 1 proximal splenic vein thrombosis (pSVT). Most of the patients were asymptomatic (n=18).
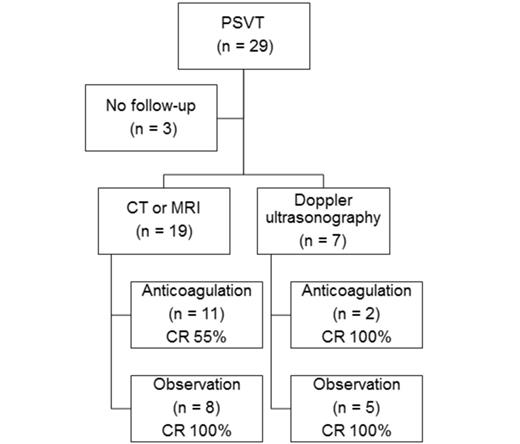
No significant association between PSVT and any clinical or biological characteristics such as platelet count, preoperative treatments, thrombocytosis, or efficacy of splenectomy was observed. However, PSVT patients tended to have higher spleen weights (206 g vs 102 g, p = 0.14). Thirteen of the 29 patients with a PVST were treated with a curative anticoagulation treatment for a mean duration of 11 weeks (range, 4-37). Among the 26 patients evaluable in follow-up, the rate of complete thrombosis resolution was 84% (21/26); specifically, 62% (8/13) in anticoagulated patients and 100% in the 13 non anticoagulated patients (9 dSVT, 4 iPVT+dSVT). A portal cavernoma occurred after iPVT+dSVT despite anticoagulation in the context of wAIHA. Anticoagulation complications included abdominal wall hematoma requiring transfusions (n=1) and iron deficiency anemia (n=1).
Conclusion
In our study, post-splenectomy PSVT was frequent and often asymptomatic, involving mostly intrahepatic portal or distal splenic veins and was resolved in half of the cases without any curative anticoagulative therapy. Our results suggest that a systematic screening of PSVT by CT scan should not be performed in absence of risk factors for thrombosis.
incidence rate and sites of PSVT.
| . | PTI, n . | AIHA, n . | Total, n . |
|---|---|---|---|
| PVST | 22/30 (73%) | 7/9 (78%) | 29/39 (74%) |
| ePVT + dSVT | 0 | 1 | 1 |
| pSVT + iPVT | 1 | 0 | 1 |
| dSVT + iPVT | 9 | 3 | 12 |
| dSVT | 11 | 3 | 14 |
| iPVT | 1 | 0 | 1 |
| . | PTI, n . | AIHA, n . | Total, n . |
|---|---|---|---|
| PVST | 22/30 (73%) | 7/9 (78%) | 29/39 (74%) |
| ePVT + dSVT | 0 | 1 | 1 |
| pSVT + iPVT | 1 | 0 | 1 |
| dSVT + iPVT | 9 | 3 | 12 |
| dSVT | 11 | 3 | 14 |
| iPVT | 1 | 0 | 1 |
outcome of anticoagulated and observed PSVT. CR = complete resolution. CT = computed tomography. MRI = magnetic resonance imaging.
outcome of anticoagulated and observed PSVT. CR = complete resolution. CT = computed tomography. MRI = magnetic resonance imaging.
Michel:AMGEN: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Roche: Research Funding; GSK: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Godeau:Roche: Research Funding; Amgen: Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal