Abstract
Introduction:
Acute myeloid leukemia (AML) is more frequent among older patients in the United States (US), with a median age at diagnosis of 67 years old. A recent case series of AML patients from India reported a median age at diagnosis of 40 years old, suggesting that the pathogenesis of AML may differ between these populations (British Journal of Haematology 2015;170:110). In this study, we examined whether differences exist in the age at diagnosis, cytogenetic risk, and overall survival (OS) of White and South Asian patients diagnosed with AML in the US.
Methods:
We used the 1973-2012 Surveillance, Epidemiology, and End Results Program (SEER) database to identify adults, age 20 years or older, diagnosed with AML between 2000 and 2012. We included patients with documented race/ethnicity and known age at diagnosis. We compared age at diagnosis, cytogenetic risk, and OS according to White or South Asian race/ethnicity, based on patient surname as defined by SEER. We stratified age at diagnosis into age groups, defined as 20-24, 25-34, 35-44, 45-54, 55-64, and >65 years old, to compare the White and South Asian populations. Using the 2012 US Census population age distributions, we directly standardized the distribution of age at diagnosis of AML in SEER, weighted according to the age distribution of the total White and South Asian populations in the US. We categorized SEER-reported cytogenetic profiles as having favorable or adverse prognosis based on accepted definitions. We compared cytogenetic risk and OS between White and South Asian populations according to stratified age group at diagnosis. Differences in age at diagnosis were calculated using the Mann-Whitney test. OS was compared by the Log-rank test and estimated by the method of Kaplan and Meier. P-values <0.05 were considered significant.
Results:
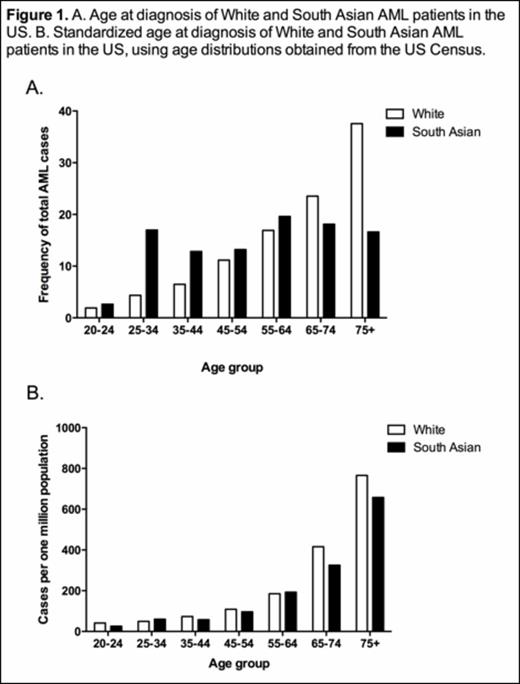
39,192 patients, age 20 years old and above, were diagnosed with AML from 2000 to 2012 and had documented race/ethnicity at diagnosis in the SEER database. South Asian patients in the US were diagnosed with AML at a significantly younger age compared to White patients (Figure 1A, median age at diagnosis of 57 vs. 69.5 years old for South Asians (n=265) vs. Whites (n=33,419), p=<0.0001). Along with younger age at diagnosis, South Asians had a greater reported frequency of favorable cytogenetic risk (17.7% vs. 9.7% favorable cytogenetic risk for South Asians vs. Whites). Analysis of the demographics of the US population also showed that the South Asian population was significantly younger than the White population (median age of 40 vs. 50 years old for South Asians (n=2,447,009) vs. Whites (n=172,366,410), p=<0.0001). Direct standardization of the age at AML diagnosis with the age distributions of White and South Asian census populations in the US abrogated the differences in age at diagnosis between these groups (Figure 1B, p=0.8718). Standardization by age distribution also narrowed the difference in favorable cytogenetic risk between Whites and South Asians (17.9 vs. 19.1 cases per one million people, respectively). OS was not different between Whites and South Asians in the 20-49 year old age group (median OS: 46 vs. 60 months for Whites (n=5,272) vs. South Asians (n=96), p=0.4986), the 50-64 year old age group (median OS: 13.5 vs. 16 months for Whites (n=6,066) vs. South Asians (n=62), p=0.5088), or the >65 year old age group (median OS: 3 vs. 4.5 months for Whites (n=13,692) vs. South Asians (n=66), p=0.8491).
Conclusions:
In the US, AML patients of South Asian descent are diagnosed at a younger age and have more favorable cytogenetic risk profiles as compared to their White counterparts, which is of epidemiologic importance. Nevertheless, these findings appear to reflect the younger age distribution of the entire South Asian population as compared to the total White population in the US, rather than a difference in the inherent biology or pathogenesis of AML. These data highlight the importance of directly standardizing age distributions in population outcomes research.
Fathi:Agios Pharmaceuticals: Other: Advisory Board participation; Merck: Other: Advisory Board participation; Seattle Genetics: Other: Advisory Board participation, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal