Abstract
Introduction: Rituximab (R) has improved outcomes in diffuse large B-cell lymphoma (DLBCL) but early complications, such as gastric perforation, have been reported (median time to event 6 days). As the role of surgery for gastric diffuse large B cell lymphoma (gDLBCL) has evolved from the primary management of the disease to the management of its complications, we sought to further define surgical trends and to explore whether the introduction of R and the decreasing rates of primary surgery influenced early mortality in patients with gDLBCL.
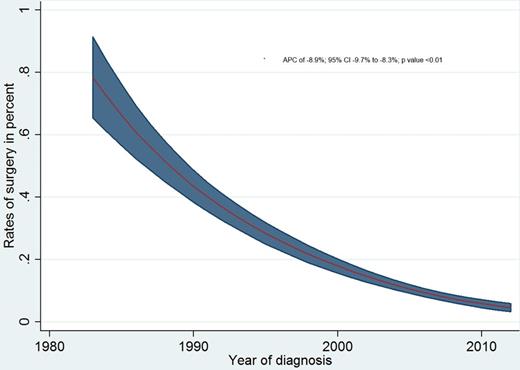
Methods: The authors utilized the Surveillance Epidemiology and End Results (SEER) 18 database (November 2014 submission) to extract relevant data on patients with gDLBCL diagnosed between 1983-2012 using the case listing session. Eligible cases of gDLBCL were identified from the SEER 13 database using a combination of International Classifications of Diseases for Oncology, 3rd edition (ICD-O-3) code for DLBCL (9680/3) and site codes for stomach (C60.x). Primary site-specific cancer directed surgery using SEER site-specific surgical codes and annual trends in the receipt of surgery among patients with gDLBCL using Joinpoint regression program were evaluated. Unadjusted percentages along with 95% confidence intervals (computed using Bootstrapping methods) were computed for each year. Changes in the trend of surgical rates were evaluated by Monte Carlo Permutation method.
We compared the impact of the introduction of R on early mortality rates in our study population. Using the year 2006, date of FDA approval for R as first-line therapy, as a cutoff, we studied the 30 and 60-day mortality rates. Multivariate logistic regression was used to study the impact of year of diagnosis (before and after 2006) on early mortality rates adjusting for age, sex, race and stage at diagnosis. The level of significance chosen was 0.05. All p-values were two sided.
Results: 5814 patients (pts) with gDLBCL were identified. There were 4124 pts diagnosed prior to 2006 and 1690 patients with gDLBCL diagnosed after 2006. Median age was 71 years (range 1 to 105 years), of which 55.5% (n=3224) were males and 80.7% (n=4694) were white. The majority of patients were Stage I (43.7%; n =2539) or Stage II (19.7%; n= 1145) at diagnosis. 16% (n=932) received any form of radiation therapy. 1088 (18.7%) received primary cancer directed surgery. Patients receiving surgery for gDLBCL declined from 63% in 1983 (34 out of 54 patients) to 8% (19 out of 250) in 2012. Joinpoint trend analysis revealed that the sharpest decline was seen between the years 2000-2010 (annual percentage change, APC -12.31; 95% confidence interval -16.8 to -7.6; p value <0.01). The adjusted rates of surgery computed using poisson regression (adjusted for age, sex, race and stage at diagnosis) declined from 54.4% in 1983 to 6.9% in 2012 with an APC of -8.9% (95% CI -9.7% to -8.3%; p value <0.01). The 30-day mortality rate prior to 2006 was 9.7% as compared to 10.3% among patients diagnosed after 2006 (p value 0.48). The 60-day mortality rate was similar in the two groups as well (16.3% versus 15.2%; p value 0.29). Multivariate logistic regression showed that the patients before and after 2006 were similar in terms of the 30-day mortality rate (OR 0.97; 95% CI 0.79-1.18; p value 0.79) and the 60-day mortality rate (OR 0.94; 95% CI 0.80-1.11; p value 0.48) after adjusting for age, gender, race and stage at diagnosis.
Conclusions: The period after the introduction of R was associated with the sharpest decline in primary cancer directed surgery for gDLBCL. While R is associated with perforation risk, no significant increase in 30 or 60-day mortality was seen in those treated after R was approved for first-line therapy. While R appears to have significantly changed how surgery is utilized in gastric DLBCL, early mortality was unchanged.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal