Abstract

Introduction
Hemophagocytic lymphohistiocytosis (HLH) is a rare, life-threatening syndrome of extreme hyperinflammation. It does not self-limit and needs to be stopped by effective treatment. This reaction can be triggered by numerous factors, including infection, malignancy and autoimmune disease. HLH used to be diagnosed in children, but in last few years more and more adults with this syndrome are treated. This raising awareness enabled creating retrospective registry of adult HLH patients in Poland.
Methods
A multicenter retrospective analysis of adult (≥18 years) patients was performed. Inclusion criteria were based on the HLH-2004 protocol.
Results
Forty four adult (median age 34, range 18-80) patients from 13 clinical centers were reported. The gender ratio was balanced (M/F: 23/21). Patients fulfilled on the average 5.2 of HLH-2004 criteria. Due to the lack of possibility of sCD25 and NK activity testing in majority of centers only 6 criteria were actually evaluated. Also 6 patients with strong clinical suspicion (e.g. recurrent HLH) fulfilling 4 out of 6 available criteria were included. The most frequent triggering factor was malignancy (14/44) with lymphoma (T-cell 6/14, B-cell 4/14) being the most common. Infection-associated HLH was present in 13 patients, most of which was attributed to EBV (11/13; additionally CMV and B19 occurred). One patient suffered from both T-lymphoma and EBV infection. The most frequent autoimmune diseases identified were Still's disease (n=3) and systemic lupus erythematosus (n=2). In 11 patients clear triggering factor could not be identified. Three patients underwent liver transplantation.
Baseline characteristics of all patients are shown in Table 1. Briefly, almost all patients presented with extreme hyperferritinemia, fever, splenomegaly. Other Important features are liver involvement and coagulopathy.
Majority of patients were treated according to HLH-2004 protocol, except of patients with malignancy treated with disease-specific chemotherapy regimens (with emphasis on inclusion of etoposide if appropriate). None of the patients underwent stem cell transplantation (SCT) as HLH therapy; one patient had HLH triggered by EBV reactivation after alloSCT.
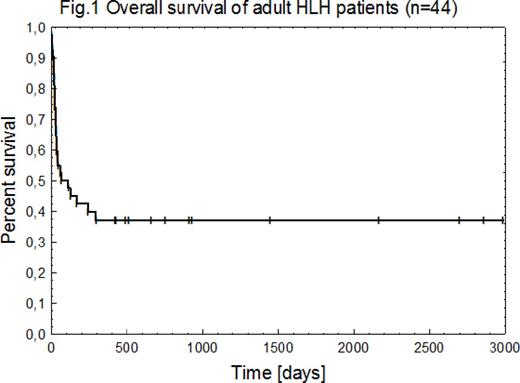
Median survival was 66 days (Fig.1), 39% of patients survived with median observation of 21 months (3-98).
Conclusions
Heterogeneity of HLH syndrome was confirmed in Polish population, with malignancy and EBV infection being the most frequent triggering factors.
Awareness of HLH in adults is raising, but it should be fostered as HLH is still underdiagnosed. Further studies are needed to deepen our knowledge about HLH in adults.
Analysis of additional, newly diagnosed cases is ongoing and will be presented at the meeting.
Baseline patient characteristics
| Characteristic . | [unit] . | (n) . | % . | Median . | Range . |
|---|---|---|---|---|---|
| Fever | (n=44) | 97.7 | |||
| Splenomegaly | (n=44) | 90.9 | |||
| Hemophagocytosis | (n=41) | 70.7 | |||
| Hyperferitinemia | [µg/l] | (n=44) | 100 | 14280 | 846-126680 |
| Hemoglobin | [g/dl] | (n=44) | 8.3 | 6.1-13.9 | |
| Neutrophil count | [G/l] | (n=41) | 1.1 | 0-173 | |
| Platelet count | [G/l] | (n=44) | 43 | 4-349 | |
| Triglycerides | [mg/dl] | (n=38) | 316 | 74-1559 | |
| Fibrinogen | [mg/dl] | (n=43) | 166 | 30-901 | |
| PT | [s] | (n=30) | 15.9 | 9-46.6 | |
| APTT | [s] | (n=39) | 36 | 22-86.8 | |
| CRP | [mg/l] | (n=40) | 40.1 | 0.4-373 | |
| LDH | [U/l] | (n=39) | 970 | 195-13160 | |
| AST | [U/l] | (n=39) | 150 | 16-16280 | |
| ALT | [U/l] | (n=40) | 100 | 18-12390 | |
| Total Bilirubin | [mg/dl] | (n=37) | 3.7 | 0.34-25.6 |
| Characteristic . | [unit] . | (n) . | % . | Median . | Range . |
|---|---|---|---|---|---|
| Fever | (n=44) | 97.7 | |||
| Splenomegaly | (n=44) | 90.9 | |||
| Hemophagocytosis | (n=41) | 70.7 | |||
| Hyperferitinemia | [µg/l] | (n=44) | 100 | 14280 | 846-126680 |
| Hemoglobin | [g/dl] | (n=44) | 8.3 | 6.1-13.9 | |
| Neutrophil count | [G/l] | (n=41) | 1.1 | 0-173 | |
| Platelet count | [G/l] | (n=44) | 43 | 4-349 | |
| Triglycerides | [mg/dl] | (n=38) | 316 | 74-1559 | |
| Fibrinogen | [mg/dl] | (n=43) | 166 | 30-901 | |
| PT | [s] | (n=30) | 15.9 | 9-46.6 | |
| APTT | [s] | (n=39) | 36 | 22-86.8 | |
| CRP | [mg/l] | (n=40) | 40.1 | 0.4-373 | |
| LDH | [U/l] | (n=39) | 970 | 195-13160 | |
| AST | [U/l] | (n=39) | 150 | 16-16280 | |
| ALT | [U/l] | (n=40) | 100 | 18-12390 | |
| Total Bilirubin | [mg/dl] | (n=37) | 3.7 | 0.34-25.6 |
PT indicates Prothrombin Time; APTT, Activated Partial Thromboplastin Time; CRP, C-Reactive Protein; LDH, lactate dehydrogenase; AST, aspartate aminotransferase; ALT, alanine aminotransferase
Knopinska-Posluszny:Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Speakers Bureau; Teva: Other: travel, accommodation, Speakers Bureau. Wiktor-Jedrzejczak:Amgen, Inc.: Research Funding; Onconova: Other: Advisory Board; Novartis: Research Funding; Pfizer: Other: Advisory Board; Roche: Other: Advisory Board, Research Funding; Jansen: Other: Advisory Board; Celgene: Other: Advisory Board.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal