Abstract
A significant number of patients with ovarian cancer develop venous thromboembolism that is associated with a worse prognosis. The etiology of an increased frequency of venous thrombosis in cancer patients is not clear, and various hypotheses, including the presence of hyperreactive platelets, have been postulated. Hyperreactive platelets have a lower threshold for aggregation, and hence there is a higher number of degranulated platelets in circulation and a higher concentration of platelet granular contents in plasma.
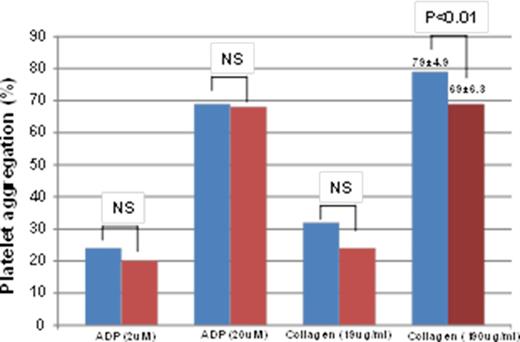
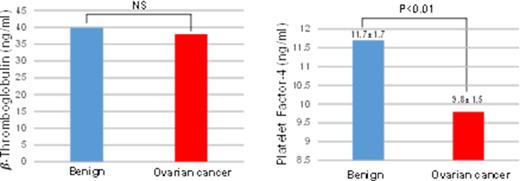
We compared ADP- and collagen-induced platelet aggregation in patients with ovarian cancer to those in patients with benign ovarian tumors. To reduce the effect of confounding factors such as surgery or chemotherapy, all blood samples were collected prior to any surgical interventions or chemotherapy. To detect hyperreactivity of platelets, we used both low and high doses of platelet agonists. To evaluate platelet preactivation at baseline, we measured the plasma concentration of b-thromboglobulin (b-TG) and platelet factor-4 (PF-4) as markers of platelet α granule secretion.
All studies were approved by the Institutional Review Boards of the University of Texas, M.D. Anderson Cancer Center. Whole blood samples were collected from 34 patients with ovarian cancer and 19 patients with benign ovarian tumors into sodium citrate anticoagulant and processed within 2 hours after collection. Platelet rich plasma (PRP) was prepared by 15 min of 850 rpm centrifugation at room temperature. Aggregation studies were conducted in a light transmission aggregometer (Bio/Data Corporation), using ADP (at 2mM and 20 mM) and collagen (at 19 mg/ml and 190 mg/ml). Platelet poor plasma (PPP) was prepared by centrifuging PRP samples at 2500 rpm for 20 min at room temperature. All PPP samples were stored at -80ºC and the quantity of b-TG and PF-4 was determined by ELISA.
We found that platelets isolated from ovarian cancer patients showed aggregation responses similar to platelets from patients with benign ovarian tumors (Figure 1). There was a statistically significant difference in the high-dose collagen-induced platelet aggregation between cancer and benign tumor samples, with increased aggregation of platelets from patients with benign tumors (79 ± 4.9%) in comparison to aggregation of platelets from cancer platelets (69 ± 6.3%). To investigate preactivation of platelets in cancer patients, we measured b-TG and PF-4 in PPP samples. We did not detect a higher concentration of b-TG and PF-4 in cancer PPP samples (Figure 2). In fact, PPP from cancer patients had a lower concentration of both α granule constituents. In the case of PF-4, the difference was statistically significant (9.8 ± 1.5 ng/ml for cancer patients versus 11.7 ± 1.7 ng/ml for patients with non-malignant tumors).
We conclude that platelets from ovarian cancer patients are not hyperreactive and are not degranulated or preactivated. Links between ovarian cancer, venous thromboembolism and platelets may be absent or may involve non-hemostatic platelet functions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal