Abstract

Background: Allogeneic SCT is considered standard treatment for patients with advanced phase CML (accelerated phase, blast crisis), de novo Ph+ ALL, or patients in chronic phase (CP) resistant or intolerant to at least 2 tyrosine kinase inhibitors (TKI). Ponatinib is FDA and EMA approved for the treatment of CML or Ph+ ALL in patients with the BCR-ABL1 T315I mutation or for whom no other TKI therapy is indicated. In patients harboring the T315I mutation, ponatinib currently represents a suitable alternative treatment option to allogeneic SCT. However, differences in outcomes between patients treated with ponatinib and allogeneic SCT have not been analyzed.
Objective: To compare overall survival (OS) among CML and Ph+ ALL patients with the BCR-ABL1 T315I mutation treated with ponatinib (in PACE) versus allogeneic SCT (in the EBMT database).
Methods: Data from a Phase II trial of ponatinib (PACE trial; Cortes et al., New Engl J Med 2013; NCT01207440) and European Bone Marrow Transplant (EBMT) registry were pooled to conduct an indirect comparison of ponatinib with allogeneic SCT. Both ponatinib and allogeneic SCT cohorts comprised patients with the T315I mutation age 18 years or older in any phase of CML or with Ph+ ALL. All patients harbored the T315I mutation detected by Sanger sequencing, DHPLC, PCR-RFLP, or other equivalent tests. Allogeneic SCT patients in their second CP phase were excluded, and no patients in the EBMT database were treated with ponatinib prior to receiving allogeneic SCT. The date of intervention (ponatinib or SCT) served as the index date. Baseline demographic and clinical characteristics were compared between the two intervention groups. OS was compared between the two groups using adjusted Kaplan-Meier (KM) survival curves and multivariate Cox proportional hazards models; all comparisons were adjusted for age (as a continuous variable), gender, geographic region (Europe, Asia, and Australia vs. North America), time from CML diagnosis to intervention, and CML phase or Ph+ ALL at intervention to control confounding by these variables. Results were presented overall and stratified by phase of CML or Ph+ ALL.
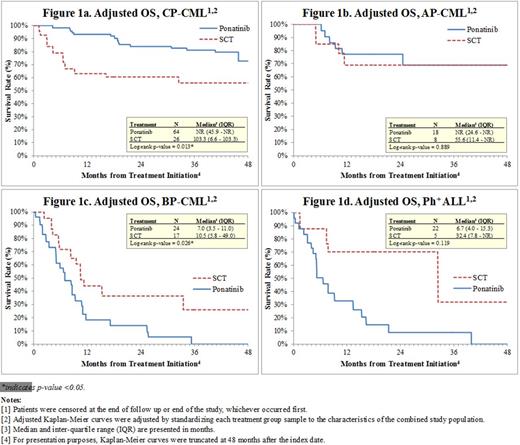
Results: A total of 184 (128 ponatinib, 56 allogeneic SCT) patients were included in the analysis: 90 were in CP-CML, 26 were in accelerated phase (AP-CML), 41 were in blast phase (BP-CML), and 27 had Ph+ ALL. On average, ponatinib patients were older than allogeneic SCT patients on the date of intervention (median age 53 vs. 45 years, p=0.006). In addition, a larger proportion of patients in the ponatinib group were from North America than in the allogeneic SCT group (43.8% vs. 26.8%, p=0.030). Median time from diagnosis to intervention was longer for patients treated with ponatinib compared with those treated with allogeneic SCT in CP-CML (58 vs. 32 months, p=0.029), but not significantly different in AP-CML (80 vs. 49 months, p=0.075) nor Ph+ ALL (17 vs. 10 months, p=0.212). This period was nominally shorter for the ponatinib cohort in BP-CML (26 vs. 43 months, p=0.340). Over 93% of patients in both treatment cohorts in all disease phases reported previous use of imatinib. Adjusted median OS was significantly longer in CP-CML patients treated with ponatinib as opposed to allogeneic SCT patients (KM median: not reached [NR] vs. 103.3 months, p=0.013), with a hazard ratio (HR) of 0.37 (95% CI: 0.16, 0.84, p=0.017). Median OS was not significantly different between the two treatment groups in patients with AP-CML (NR vs. 55.6 months, p=0.889; HR=0.90 [95% CI: 0.20, 4.10, p=0.889]). However, among patients with BP-CML, ponatinib was associated with significantly shorter OS compared with allogeneic SCT: median 7.0 vs. 10.5 months (p=0.026), HR=2.29 (95% CI: 1.08, 4.82, p=0.030). Ph+ ALL patients treated with ponatinib had nominally shorter median OS than allogeneic SCT (6.7 vs. 32.4 months, p=0.119; HR=2.77 [95% CI: 0.73, 10.56, p=0.136]). See Figures 1a-1d for adjusted KM survival curves.
Conclusion: AllogeneicSCT remains a potential curative therapy for patients with BP-CML. However, ponatinib was associated with significantly longer OS than allogeneic SCT in patients with CP-CML that harbor the T315I mutation and could represent a promising therapeutic alternative in this setting, although follow-up remains short to date. OS was similar between intervention groups in AP-CML and longer for allogeneic SCT patients in BP-CML and Ph+ ALL.
Nicolini:Ariad Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Basak:MSD: Consultancy, Honoraria; Astellas: Honoraria; Sanofi: Honoraria; Pierre-Fabre: Honoraria. Kim:Pfizer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Il-Yang: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Pinilla-Ibarz:BMS: Consultancy, Speakers Bureau; Novartis: Consultancy; ARIAD: Consultancy; Pfizer: Consultancy, Speakers Bureau. Apperley:ARIAD: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Hughes:Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding; ARIAD: Honoraria, Research Funding. Niederwieser:Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Mauro:Ariad: Consultancy; Pfizer: Consultancy; Novartis Pharmaceutical Corporation: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy. Chuah:Bristol-Myers Squibb: Honoraria; Novartis: Honoraria; Chiltern International: Honoraria. Hochhaus:Pfizer: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; ARIAD: Honoraria, Research Funding. Martinelli:Novartis: Consultancy, Speakers Bureau; MSD: Consultancy; Pfizer: Consultancy; Ariad: Consultancy; ROCHE: Consultancy; BMS: Consultancy, Speakers Bureau; AMGEN: Consultancy. DerSarkissian:ARIAD: Research Funding. Kageleiry:ARIAD: Research Funding. Yang:ARIAD: Employment. Huang:ARIAD: Employment, Equity Ownership. McGarry:ARIAD: Employment, Equity Ownership. Cortes:Pfizer: Consultancy, Research Funding; BMS: Consultancy, Research Funding; BerGenBio AS: Research Funding; Teva: Research Funding; Novartis: Consultancy, Research Funding; Ariad: Consultancy, Research Funding; Astellas: Consultancy, Research Funding; Ambit: Consultancy, Research Funding; Arog: Research Funding; Celator: Research Funding; Jenssen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal