Abstract
Introduction
In pre-rituximab era, the IPI has been developed and widely used to predict the prognosis of aggressive lymphoma while Miller's stage modified IPI1 was reported as a better prognostic model for limited stage DLBCL. Recently, NCCN-IPI2 was stated to be a better predictor of prognosis for DLBCL in rituximab era. We aim to compare the prognostic significance between IPI, Miller's stage modified IPI, NCCN-IPI and the new proposed stage adjusted IPI (St-IPI) in limited stage DLBCL patients treated with rituximab based regimens.
Methods
From the 4,371 patients in a multi-institutional registry of newly diagnosed lymphoma in Thailand between 2007-2014, there were a total of 2,399 patients with DLBCL. We included patients with limited stage DLBCL receiving R-CHOP or R-CHOP-liked chemotherapy. The clinical outcomes were analyzed according to IPI, Miller's stage modified IPI, NCCN-IPI and St-IPI. To generate the St-IPI, we used 3 predictors from IPI namely, age > 60, elevated LDH and ECOG ≥ 2, classified patients into 3 risk cohorts, i.e., the low (score 0), intermediate (score 1-2), and high risk (score 3) group.
Results
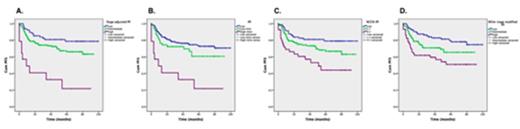
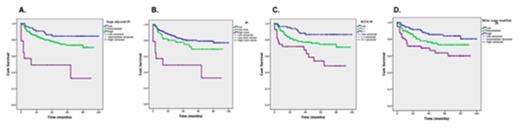
A total of 274 patients with a median age of 58 years (range, 15-91) were included. Seventy-four percent of the cohort had stage II disease, 44% and 32% of them had elevated LDH and ECOG ≥ 2, respectively. According to St-IPI, 77, 183 and 14 patients were categorized as low (score 0), intermediate (score 1-2) and high risk groups (score 3), respectively. Most of the patients (96%) received R-CHOP regimen and one fifth of them underwent consolidation radiotherapy, contributing to a complete response rate of 76%. With a median follow up of 52 months, the 5-year progression free survival (PFS) according to St-IPI among low, intermediate and high risk groups were 79%, 66% and 22%, respectively (HR 2.48, 95%CI: 1.55-3.86). The corresponding figures for 5-year overall survival (OS) were 84%, 73% and 49%, respectively (HR 2.95, 95%CI: 1.54-4.37). The 5-year PFS and OS according to IPI, NCCN-IPI and Miller's stage modified IPI were described in Table 1. When comparing between risk models, St-IPI was able to discriminate more accurately low risk PFS than IPI, distinguished more precisely high risk PFS than NCCN-IPI and Miller's stage modified IPI (Figure 1). All risk models had no differences in predicting OS at 5 years, nevertheless, there was a trend of inferior survivals after 5 years among limited stage DLBCL patients with high risk St-IPI (Figure 2).
Conclusion
St-IPI is a simple and better model in predicting PFS for limited stage DLBCL treated with R-CHOP. The model is able to predict the lower risk disease more discriminately than the IPI which would suggest the tailor therapy approach to avoid unnecessary treatment related toxicities. Moreover, the St-IPI is better in predicting patients with high risk of relapses in whom more aggressive treatment is warranted to improve the cure rate of the patients.
1 Miller, et al. N Engl J Med 1998; 339: 21-6
2 Zhou, et al. Blood. 2014;123: 837-842
5-year PFS and OS according to risk groups categorized by St-IPI, IPI, NCCN-IPI and Miller's stage modified IPI
| Risk model . | 5-year PFS (%) . | HR (95%CI) . | P -value . | 5-year OS (%) . | HR (95%CI) . | P -value . |
|---|---|---|---|---|---|---|
| St-IPI (Age > 60, elevated serum LDH, ECOG ≥ 2) | 2.48 (1.55-3.86) | <0.001 | 2.95 (1.54-4.37) | <0.001 | ||
| Low (score 0, n= 77) | 79 | 84 | ||||
| Intermediate (score 1-2, n=183) | 66 | 73 | ||||
| High (score 3, n=14) | 22 | 49 | ||||
| IPI (Age > 60, elevated LDH, ECOG ≥ 2, Stage ≥ III, extranodal involvement >1) | 1.99 (1.43-2.78) | <0.001 | 2.03 (1.40-2.97) | <0.001 | ||
| Low (score 0-1, n =203) | 73 | 79 | ||||
| Low-intermediate (score 2, n=57) | 61 | 69 | ||||
| High-intermediate (score 3, n=14) | 22 | 49 | ||||
| High (score 4-5, n=0) | - | - | ||||
| NCCN-IPI (Age ≤40, >40-60, 60-75, >75; elevated serum LDH 1-3X, > 3X; ECOG ≥ 2, Stage ≥ III, extranodal disease in bone marrow, liver/GI tract or lung) | 1.83 (1.30-2.57) | <0.001 | 2.13 (1.45-3.13) | <0.001 | ||
| Low (score 0-1, n=82) | 79 | 86 | ||||
| L-I (score 2-3, n=152) | 67 | 74 | ||||
| H-I (score 4-5, n=40) | 44 | 54 | ||||
| High (score ≥ 6, n=0) | - | - | ||||
| Miller's stage modified IPI (Age > 60, elevated serum LDH, ECOG ≥ 2, Stage II) | 1.71 (1.28-2.28) | <0.001 | 1.69 (1.22-2.35) | 0.02 | ||
| Low (score 0-1, n=107) | 78 | 84 | ||||
| Intermediate (score 2, n=109) | 65 | 73 | ||||
| High (score 3-4, n=58) | 51 | 49 |
| Risk model . | 5-year PFS (%) . | HR (95%CI) . | P -value . | 5-year OS (%) . | HR (95%CI) . | P -value . |
|---|---|---|---|---|---|---|
| St-IPI (Age > 60, elevated serum LDH, ECOG ≥ 2) | 2.48 (1.55-3.86) | <0.001 | 2.95 (1.54-4.37) | <0.001 | ||
| Low (score 0, n= 77) | 79 | 84 | ||||
| Intermediate (score 1-2, n=183) | 66 | 73 | ||||
| High (score 3, n=14) | 22 | 49 | ||||
| IPI (Age > 60, elevated LDH, ECOG ≥ 2, Stage ≥ III, extranodal involvement >1) | 1.99 (1.43-2.78) | <0.001 | 2.03 (1.40-2.97) | <0.001 | ||
| Low (score 0-1, n =203) | 73 | 79 | ||||
| Low-intermediate (score 2, n=57) | 61 | 69 | ||||
| High-intermediate (score 3, n=14) | 22 | 49 | ||||
| High (score 4-5, n=0) | - | - | ||||
| NCCN-IPI (Age ≤40, >40-60, 60-75, >75; elevated serum LDH 1-3X, > 3X; ECOG ≥ 2, Stage ≥ III, extranodal disease in bone marrow, liver/GI tract or lung) | 1.83 (1.30-2.57) | <0.001 | 2.13 (1.45-3.13) | <0.001 | ||
| Low (score 0-1, n=82) | 79 | 86 | ||||
| L-I (score 2-3, n=152) | 67 | 74 | ||||
| H-I (score 4-5, n=40) | 44 | 54 | ||||
| High (score ≥ 6, n=0) | - | - | ||||
| Miller's stage modified IPI (Age > 60, elevated serum LDH, ECOG ≥ 2, Stage II) | 1.71 (1.28-2.28) | <0.001 | 1.69 (1.22-2.35) | 0.02 | ||
| Low (score 0-1, n=107) | 78 | 84 | ||||
| Intermediate (score 2, n=109) | 65 | 73 | ||||
| High (score 3-4, n=58) | 51 | 49 |
PFS according to risk groups categorized by St-IPI (Figure 1A), IPI (Figure 1B), NCCN-IPI (Figure 1C) and Miller's stage modified IPI (Figure 1D)
PFS according to risk groups categorized by St-IPI (Figure 1A), IPI (Figure 1B), NCCN-IPI (Figure 1C) and Miller's stage modified IPI (Figure 1D)
OS according to risk groups categorized by St-IPI (Figure 2A), IPI (Figure 2B), NCCN-IPI (Figure 2C) and Miller's stage modified IPI (Figure 2D)
OS according to risk groups categorized by St-IPI (Figure 2A), IPI (Figure 2B), NCCN-IPI (Figure 2C) and Miller's stage modified IPI (Figure 2D)
Khuhapinant:Roche: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal