Abstract
Follicular lymphoma (FL) is a low-grade B-cell lymphoma, and the response of FL to treatment, as well as progression-free survival and overall survival (OS), are improved by the application of combined chemotherapy with rituximab (R). The cyclophosphamide, adriamycin, vincristine, and prednisolone with rituximab (R-CHOP) regimen is the standard first-line therapy for patients with FL. However, many patients have coexistent diseases (comorbidities), and it is believed that therapeutic decision-making is influenced by comorbidities. In this study, we retrospectively analyzed treatment decision-making and its outcome for patients with FL. Based on this analysis, we investigated how the presence of comorbidity affects the survival of patients with FL.
We analyzed 113 patients who were diagnosed with FL at our institute between September 2001 and March 2014. The treatment strategy was classified as observation without treatment, chemotherapy, radiotherapy, and others. Chemotherapy was subclassified as R-CHOP, reduced R-CHOP (the chemotherapeutic dose was reduced), and other chemotherapy. The severity of the comorbidity present at the time of diagnosis of FL was estimated according to the Charlson Comorbidity Index (CCI) (Table 1).
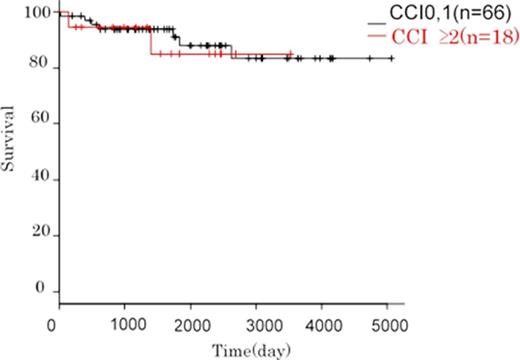
The clinical characteristics of the 113 patients are shown in Table 2. The median age of the patients was 60 years. Six patients were observed without treatment, and 8 patients underwent resection or localized radiation for lymphoma. R-CHOP and other chemotherapy regimens were utilized in 84, and 15 patients, respectively. The 5-year OS rates of patients treated with R-CHOP, reduced R-CHOP, and other chemotherapy regimens were 92.3%, 75.5%, and 74.1%, respectively. As shown in a previous study (Andre Wieringa, et al., Br J Haematol, 2014, 165, 489-496), the 5-year OS rate of patients with CCI score ≥2 was inferior to that of patients with CCI 0-1 (CCI ≥2 (n = 32); 76.5%, CCI 0-1(n=81); 92.4%, p = 0.0361, Figure 1a). When we analyze the patients treated with R-CHOP, the overall response rate was 92.4% (complete response [CR] = 77.2%, partial response [PR] = 15.1%) in patients with a CCI score of 0-1 and 94.4% (CR = 77.8%, PR = 16.7%) in those with CCI score ≥ 2. In addition, there was no significant difference in the 5-year OS rate between patients with a CCI score of 0-1 or ≥2 (91.0% vs. 85.0%, p = 0.779, Figure 1b). Although, the percentage of patients with CCI ≥2 is lower than that of the other therapies (CCI ≥2; R-CHOP 25%, other chemotherapy 67%), it is supposed that R-CHOP is effective even if the patients have severe comorbidities. In 6 patients among these, treatment was discontinued or the chemotherapeutic dose was reduced due to myelosuppression during the designated course of therapy .The 5-year OS rate of these patients was favorable, even among those with high CCI score(CCI 0,1; 94.1%, CCI ≥2; 100%). Thus, it appears that R-CHOP with appropriate dose modification during the designated course will improve patient survival. Our results indicate that patients with severe comorbidities can be treated effectively by adjusting R-CHOP.
The items used to estimate the Charlson comorbidity index in each patient
| Comorbidity . | Score . | No. of patients . |
|---|---|---|
| Cardiac disease | 1 | 5 |
| Peripheral vascular disease | 1 | 1 |
| Cerebrovascular disease | 1 | 3 |
| Chronic pulmonary disease | 1 | 6 |
| Connective tissue disease | 1 | 8 |
| Ulcers | 1 | 3 |
| Mild liver disease | 1 | 4 |
| Diabetes | 1 | 16 |
| Tumors | 2 | 22 |
| Moderate or severe liver disease | 3 | 1 |
| Metastatic solid tumors | 6 | 2 |
| Comorbidity . | Score . | No. of patients . |
|---|---|---|
| Cardiac disease | 1 | 5 |
| Peripheral vascular disease | 1 | 1 |
| Cerebrovascular disease | 1 | 3 |
| Chronic pulmonary disease | 1 | 6 |
| Connective tissue disease | 1 | 8 |
| Ulcers | 1 | 3 |
| Mild liver disease | 1 | 4 |
| Diabetes | 1 | 16 |
| Tumors | 2 | 22 |
| Moderate or severe liver disease | 3 | 1 |
| Metastatic solid tumors | 6 | 2 |
Clinical characteristics of the patients
| Characteristic . | . | No. of patients (n = 113) . | Percentage (%) . |
|---|---|---|---|
| Sex | |||
| Male | 53 | 47 | |
| Female | 60 | 53 | |
| Age | |||
| >60 years | 56 | 50 | |
| ≤60 years | 57 | 50 | |
| IPI | |||
| Low | 55 | 49 | |
| Low-intermediate | 38 | 34 | |
| High-intermediate | 17 | 15 | |
| High | 3 | 2 | |
| FLIPI | |||
| Low | 41 | 36 | |
| Intermediate | 36 | 32 | |
| High | 36 | 32 | |
| Therapy | |||
| None | 6 | 4 | |
| Resection only | 3 | 3 | |
| Radiotherapy only | 3 | 3 | |
| Resection and radiotherapy | 2 | 2 | |
| R-CHOP | 71 | 63 | |
| Discontinued or dose was reduced | 23 | 20 | |
| Reduced R-CHOP | 13 | 12 | |
| Other chemotherapy | 15 | 13 | |
| Characteristic . | . | No. of patients (n = 113) . | Percentage (%) . |
|---|---|---|---|
| Sex | |||
| Male | 53 | 47 | |
| Female | 60 | 53 | |
| Age | |||
| >60 years | 56 | 50 | |
| ≤60 years | 57 | 50 | |
| IPI | |||
| Low | 55 | 49 | |
| Low-intermediate | 38 | 34 | |
| High-intermediate | 17 | 15 | |
| High | 3 | 2 | |
| FLIPI | |||
| Low | 41 | 36 | |
| Intermediate | 36 | 32 | |
| High | 36 | 32 | |
| Therapy | |||
| None | 6 | 4 | |
| Resection only | 3 | 3 | |
| Radiotherapy only | 3 | 3 | |
| Resection and radiotherapy | 2 | 2 | |
| R-CHOP | 71 | 63 | |
| Discontinued or dose was reduced | 23 | 20 | |
| Reduced R-CHOP | 13 | 12 | |
| Other chemotherapy | 15 | 13 | |
IPI, international prognostic index; FLIPI, follicular lymphoma international prognostic index; R-CHOP, cyclophosphamide, adriamycin, vincristine, and prednisolone with rituximab
Overall survival of patients treated with the cyclophosphamide, adriamycin, vincristine, and prednisolone with rituximab (R-CHOP) regimen according to the Charlson Comorbidity Index (CCI)
Overall survival of patients treated with the cyclophosphamide, adriamycin, vincristine, and prednisolone with rituximab (R-CHOP) regimen according to the Charlson Comorbidity Index (CCI)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal