Abstract
Background/Rationale: Success of allogeneic hematopoietic cell transplantation (HCT) is limited due to graft-versus-host disease (GvHD) and leukemia relapse. Contrary to small molecule immunosuppressive drugs like cyclosporine or methotrexate, rabbit antithymocyte globulin (ATG) used for GvHD prophylaxis with myeloablative HCT conditioning does not increase relapse. The mechanism of the anti-GvHD effect of ATG has been studied extensively, however, the reason for ATG not increasing relapse is not known. We hypothesized that ATG has an anti-leukemic activity. Here we investigated the anti-leukemic activity of ATG in vitro at concentrations achieved in vivo with our standard ATG dose of 4.5 mg/kg (median 10 mg per liter of serum; range, 1-25). We focused on complement-dependent cytotoxicity (CDC) and complement-independent cytotoxicity (CIC).
Methods: Blood or bone marrow from patients newly diagnosed with acute myeloid leukemia (AML, n=25) or acute lymphoid leukemia (ALL, n=4), obtained before induction chemotherapy, was used as the source of leukemic cells. We measured CDC and CIC of ATG, specifically against leukemic blasts at clinically achieved concentrations (1-25 mg/L) and an achievable concentration (50 mg/L). The leukemic blasts were identified as CD45dim/neg and side scatter low (SSclow) cells in case of AML-M0, M1 or M2 (according to British-American-French classification) or ALL. In case of AML-M4 or M5, we gated on CD45dim/neg and SSclow/intermediate cells. These cells could contain both leukemic and normal blasts and some post-blast (maturing/mature) cells. We minimized the fraction of normal blasts and post-blast cells included by introducing a "dump channel". The dump channel consisted of antibodies against antigens expressed by cells of lineages other than the leukemia lineage (except for antigens aberrantly expressed by the leukemic cells) and by post-blast cells. For most AML patients, the dump channel consisted of CD10, CD19, CD41a, CD235a, CD14 and CD16. For most ALL patients, the dump channel consisted of CD117, CD33, CD41a, CD235a, CD14 and CD16. Thus, leukemic blasts were defined as mononuclear cells that were CD45dim/neg and SSclow (or SSclow/intermediate for M4/M5) and did not express dump channel antigens. CDC was induced by incubation of the patient specimen with human serum (source of complement). CIC was induced by incubation of the patient specimen with heat-inactivated serum (no complement). For CDC dead cells were identified as 7-amino-actinomycin D positive (7AAD+). For CIC dead/dying cells were identified as Annexin V positive (Annexin V+).
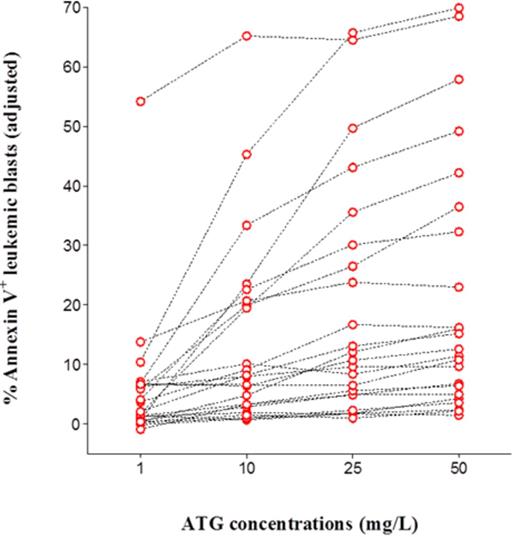
Results: ATG induced death of leukemic blasts both via CDC and CIC. Median 0.3%, 3.0%, 12.6% and 41.7% blasts were killed with 1, 10, 25 and 50 mg/L ATG, respectively, via CDC. Median 2.1%, 8.0%, 11.4% and 12.6% blasts were killed after 4 hour incubation with 1, 10, 25 and 50 mg/L ATG, respectively, via CIC. For both CDC and CIC, the percents were significantly higher than background (p<0.05). There was a high variability in the sensitivity of the leukemic blasts to ATG. The adjusted (background subtracted) percent of blasts killed ranged from 2.6% to 93.8% via CDC (Figure 1) and from 1.5% to 69.9% via CIC (Figure 2). When we arbitrarily defined a patient with resistant leukemic blasts as <10% (adjusted) leukemic blasts dead after exposure to 50 mg/L ATG, there were 3/28 patients with resistant leukemic blasts in case of CDC (Figure 1) and 9/23 patients in case of CIC (Figure 2).
Conclusion: ATG at clinically relevant concentrations kills primary leukemic blasts in vitro. Some acute leukemias are highly sensitive and others relatively resistant to ATG. Whether this applies to in vivo needs to be determined. If yes, and given that the killing of leukemic cells is ATG concentration-dependent, conditioning regimens with high dose ATG could be developed for patients with leukemia sensitive to ATG to maximize the concurrent anti-GvHD and anti-relapse effects.
Sensitivity of leukemic blasts to ATG induced CDC is highly variable. Percents 7AAD+ (dead) leukemic blasts shown are adjusted percents. In case of a negative value of the adjusted percent, zero value is displayed here.
Sensitivity of leukemic blasts to ATG induced CDC is highly variable. Percents 7AAD+ (dead) leukemic blasts shown are adjusted percents. In case of a negative value of the adjusted percent, zero value is displayed here.
Sensitivity of leukemic blasts to ATG induced CIC is highly variable. Percents Annexin V+ (dying or dead) leukemic blasts shown are adjusted percents. In case of a negative value of the adjusted percent, zero value is displayed here.
Sensitivity of leukemic blasts to ATG induced CIC is highly variable. Percents Annexin V+ (dying or dead) leukemic blasts shown are adjusted percents. In case of a negative value of the adjusted percent, zero value is displayed here.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal