Abstract
Background
Splenomegaly is a common finding in general medical patients. The cause of splenomegaly is often found outside the spleen and therefore an extensive diagnostic medical work-up is frequently required. There is very little data on the distribution of causal diagnoses and, to the best of our knowledge, accurate data on the risk of hematological malignancies, hepatic diseases and storage diseases among patients with splenomegaly have never been reported. The aim of this pilot study is to investigate the validity of the splenomegaly ICD-10 diagnoses, in order to ascertain if a nationwide registry study of the above stated risks can be undertaken, and to investigate which causal diagnoses are most common.
Method
The study was conducted as a cohort with data from the Danish health care system. Patients with an ICD-10 diagnosis of splenomegaly at Odense University Hospital (OUH) from January 1st 1994 to December 31st 2013 were identified through the Danish National Registry of Patients (DNRP). Patients with a known diagnosis of a malignant hematological disease, liver cirrhosis, or splenomegaly before January 1st 1994 were excluded. The clinical records from OUH provided data, and splenomegaly was, in accordance with current literature, defined as; 1. clinically palpable spleen by abdominal examination on two occasions or by two physicians on the same occasion, 2. the longest diameter being ≥13 cm by ultrasonography or >10 cm by computed tomography or 3. wet weight >291g at excision or autopsy. The analyses presented in this abstract are interim analyses.
Results
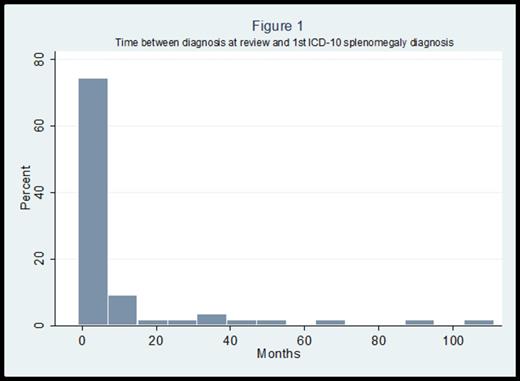
At the time of analysis 65 out of 132 (49.2%) medical records had been reviewed. Two patients with diagnoses of chronic myeloproliferative neoplasms prior to 1994 were excluded. The mean age of the population at the time of splenomegaly diagnosis was 55 years. 63% of the patients were males and 37% were females. In 56 of the 63 patients the splenomegaly diagnosis was considered valid, the positive predictive value (PPV) was 88.9% (95% CI: 78.4, 95.4). The mean time from confirmation of splenomegaly until it was coded was 10 months; distribution can be seen in figure 1. The most common method for determining enlarged spleen, as seen in table 1, was ultrasonic imaging. Table 2 shows that hematological diseases was the most common underlying causal disease group (50%), followed by hepatic diseases (25%), other diseases (12.5%) and idiopathic causes (12.5%). Lymphomas was the single most common causal diagnosis (n=12) and liver cirrhosis the second most common (n=9).
Conclusion
The high PPV indicates that the ICD-10 splenomegaly diagnosis is valid and together with the relatively short delay of coding it indicates that registry information could be used in future studies to estimate risks of hematological malignancies, liver cirrhosis and storage diseases among patients with an enlarged spleen.
Methods of Determining Splenomegaly
| . | (n = 56) . | (%) . |
|---|---|---|
| Method | ||
| Palpable | 4 | 7.1 |
| ≥13 cm by US | 33 | 58.9 |
| >10 cm by CT | 16 | 28.6 |
| ≥13 cm by other method of scanning | 2 | 3.6 |
| >291 g by excision or autopsy | 1 | 1.8 |
| Total | 56 | 100 |
| . | (n = 56) . | (%) . |
|---|---|---|
| Method | ||
| Palpable | 4 | 7.1 |
| ≥13 cm by US | 33 | 58.9 |
| >10 cm by CT | 16 | 28.6 |
| ≥13 cm by other method of scanning | 2 | 3.6 |
| >291 g by excision or autopsy | 1 | 1.8 |
| Total | 56 | 100 |
Underlying Causes of Splenomegaly
| Diagnostic group . | Hepatic . | Hematologic . | Other . | Unknown . | Total . |
|---|---|---|---|---|---|
| Disease | |||||
| Lymphoma | - | 12 | - | - | 12 |
| MPN | - | 7 | - | - | 7 |
| CLL/HCL | - | 4 | - | - | 4 |
| Hemolytic disease | - | 1 | - | - | 1 |
| Other hematological disease | - | 4 | - | - | 4 |
| Other cancer | 1 | - | - | - | 1 |
| Liver cirrhosis | 9 | - | - | - | 9 |
| Portal hypertension | 3 | - | - | - | 3 |
| Other liver disease | 1 | - | - | - | 1 |
| Infection | - | - | 3 | - | 3 |
| Inflammatory disease | - | - | 1 | - | 1 |
| Primary splenic | - | - | 1 | - | 1 |
| Other disease | - | - | 2 | - | 2 |
| Unknown/idiopathic | - | - | - | 7 | 7 |
| Total, n | 14 | 28 | 7 | 7 | 56 |
| Total, % | 25.0 | 50.0 | 12.5 | 12.5 | 100.0 |
| Diagnostic group . | Hepatic . | Hematologic . | Other . | Unknown . | Total . |
|---|---|---|---|---|---|
| Disease | |||||
| Lymphoma | - | 12 | - | - | 12 |
| MPN | - | 7 | - | - | 7 |
| CLL/HCL | - | 4 | - | - | 4 |
| Hemolytic disease | - | 1 | - | - | 1 |
| Other hematological disease | - | 4 | - | - | 4 |
| Other cancer | 1 | - | - | - | 1 |
| Liver cirrhosis | 9 | - | - | - | 9 |
| Portal hypertension | 3 | - | - | - | 3 |
| Other liver disease | 1 | - | - | - | 1 |
| Infection | - | - | 3 | - | 3 |
| Inflammatory disease | - | - | 1 | - | 1 |
| Primary splenic | - | - | 1 | - | 1 |
| Other disease | - | - | 2 | - | 2 |
| Unknown/idiopathic | - | - | - | 7 | 7 |
| Total, n | 14 | 28 | 7 | 7 | 56 |
| Total, % | 25.0 | 50.0 | 12.5 | 12.5 | 100.0 |
Curovic Rotbain:Genzyme: Research Funding. Lund Hansen:Genzyme: Research Funding. Frederiksen:Genzyme: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal