Abstract
Introduction:
Survival among patients diagnosed with chronic myeloid leukemia (CML) has markedly improved with the advent of tyrosine kinase inhibitors. Nonetheless, access to care, including medication cost and adherence, may be barriers to therapeutic effectiveness. We performed a population-based analysis to determine if insurance status at the time of CML diagnosis influenced patient outcomes.
Methods:
We used the Surveillance, Epidemiology, and End Results Program (SEER) database (November 2014 submission) to identify patients age 15 or older, diagnosed with CML between 2007 and 2012 (SEER ICD-O3 recodes 9863 and 9875). We included patients with documented insurance status at diagnosis and categorized them as either private insurance, Medicaid coverage, or uninsured. We excluded patients with unknown insurance status at diagnosis. The primary outcome was overall survival according to insurance status. We performed a stratified analysis looking at patients age 15-64 and patients 65 or older; we did not include uninsured patients over age 65 in the analysis (n=16) due to Medicare eligibility. Covariates of interest in multivariable analysis included age at diagnosis, race, ethnicity, sex, and marital status at diagnosis. Overall survival was compared by log-rank test and estimated by the method of Kaplan and Meier. P-values were significant to the 2-sided 0.05 level.
Results:
5784 patientswere diagnosed with CML between 2007 and 2012 and had insurance status documented at diagnosis. Of patients age 15-64, uninsured and Medicaid patients were younger, more often non-white race and Hispanic ethnicity, and less often married (Table 1). Over age 65, Medicaid patients were more often female, non-white race and Hispanic ethnicity, and less often married.
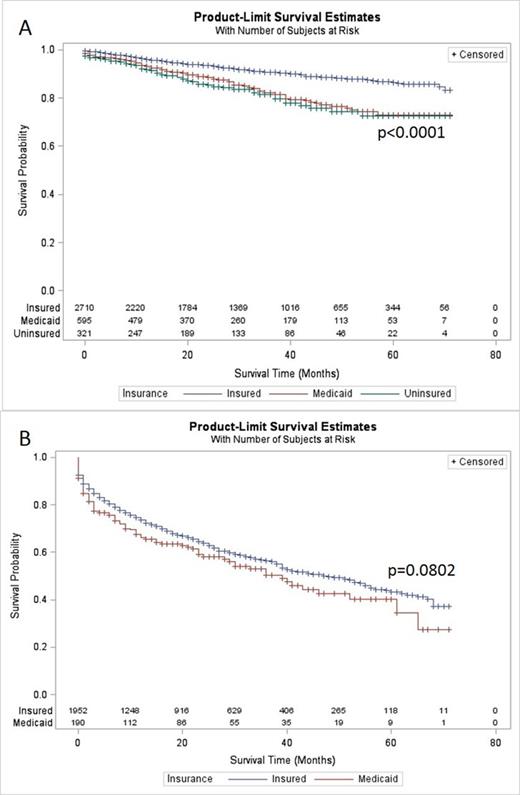
Median follow up was 32 months. Among patients age 15 to 64, being uninsured or having Medicaid was associated with worse survival compared to insured patients (5-year OS uninsured 72.7%, Medicaid 73.1%, insured 86.6%, p<0.0001) (Figure 1A). For patients over age 65, there was no difference in 5-year OS between patients with Medicaid and those with other insurance (40.2% vs. 43.4%, p=0.0802).
In multivariable analysis of patients age 15-64, compared to insured patients, there was increased mortality among patients who were uninsured (HR 2.156, p<0.0001) or on Medicaid (HR 1.972, p<0.0001). There was worse survival with increased age (HR 1.046 per year, p<0.0001), male sex (HR 1.282, p=0.0279) and, compared to married persons, being single (HR 1.883, p<0.0001). For patients over age 65 at diagnosis, only age was associated with increased mortality (HR 1.078 per year, p<0.0001).
Conclusions:
CML patients under age 65 without insurance or with Medicaid had significantly worse survival compared to patients with insurance. This difference was not noted with patients over age 65; whose survival was relatively poorer regardless of insurance status, as previously described (Cancer 2013;119:2620). Marital status and race/ethnicity also impacted survival. Despite highly effective therapies currently available for CML, these findings suggest that many patients may not have access to or receive appropriate care, in part related to insurance coverage.
Patient Demographics
| . | Age 15-64 . | p-value . | Age 65+ . | p-value . | |||
|---|---|---|---|---|---|---|---|
| (3626 patients) | (2142 patients) | ||||||
| Uninsured | Medicaid | Insured | Medicaid | Insured | |||
| Total, n (%) | 321 (8.9%) | 595 (16.4%) | 2710 (74.7%) | 190 (8.9%) | 1952 (91.1%) | ||
| Age, median (range) | 44 (18-64) | 45 (15-64) | 50 (15-64) | <0.0001 | 75 (65-97) | 76 (65-102) | 0.5388 |
| Gender, n (%) | 0.0482 | 0.0074 | |||||
| Male | 203 (63%) | 328 (55%) | 1603 (59%) | 86 (45%) | 1087 (56%) | ||
| Female | 118 (37%) | 267 (45%) | 1107 (41%) | 105 (55%) | 865 (44%) | ||
| Race, n (%) | <0.0001 | <0.0001 | |||||
| White | 231 (72%) | 402 (68%) | 2112 (78%) | 131 (69%) | 1724 (89%) | ||
| Black | 68 (21%) | 114 (19%) | 313 (12%) | 26 (14%) | 144 (7%) | ||
| American Indian | 2 (1%) | 25 (4%) | 13 (0.5%) | 2 (1%) | 7 (0.4%) | ||
| Asian, Pacific Islander | 15 (5%) | 48 (8%) | 215 (8%) | 30 (16%) | 65 (3%) | ||
| Unknown | 5 (2%) | 6 (1%) | 57 (2%) | 1 (0.5%) | 12 (0.6%) | ||
| Hispanic Ethnicity, n (%) | <0.0001 | <0.0001 | |||||
| Non- | 234 (73%) | 420 (71%) | 2341 (86%) | 151 (79%) | 1813 (93%) | ||
| Hispanic | |||||||
| Hispanic | 87 (27%) | 175 (29%) | 369 (14%) | 39 (21%) | 139 (7%) | ||
| Marital Status, n (%) | <0.0001 | <0.0001 | |||||
| Single | 141 (46%) | 281 (50%) | 588 (23%) | 41 (23%) | 153 (9%) | ||
| Married/partner | 123 (40%) | 194 (34%) | 1652 (65%) | 67 (37%) | 1069 (59%) | ||
| Divorced/separated/widowed | 45 (15%) | 90 (16%) | 288 (11%) | 72 (40%) | 578 (32%) | ||
| . | Age 15-64 . | p-value . | Age 65+ . | p-value . | |||
|---|---|---|---|---|---|---|---|
| (3626 patients) | (2142 patients) | ||||||
| Uninsured | Medicaid | Insured | Medicaid | Insured | |||
| Total, n (%) | 321 (8.9%) | 595 (16.4%) | 2710 (74.7%) | 190 (8.9%) | 1952 (91.1%) | ||
| Age, median (range) | 44 (18-64) | 45 (15-64) | 50 (15-64) | <0.0001 | 75 (65-97) | 76 (65-102) | 0.5388 |
| Gender, n (%) | 0.0482 | 0.0074 | |||||
| Male | 203 (63%) | 328 (55%) | 1603 (59%) | 86 (45%) | 1087 (56%) | ||
| Female | 118 (37%) | 267 (45%) | 1107 (41%) | 105 (55%) | 865 (44%) | ||
| Race, n (%) | <0.0001 | <0.0001 | |||||
| White | 231 (72%) | 402 (68%) | 2112 (78%) | 131 (69%) | 1724 (89%) | ||
| Black | 68 (21%) | 114 (19%) | 313 (12%) | 26 (14%) | 144 (7%) | ||
| American Indian | 2 (1%) | 25 (4%) | 13 (0.5%) | 2 (1%) | 7 (0.4%) | ||
| Asian, Pacific Islander | 15 (5%) | 48 (8%) | 215 (8%) | 30 (16%) | 65 (3%) | ||
| Unknown | 5 (2%) | 6 (1%) | 57 (2%) | 1 (0.5%) | 12 (0.6%) | ||
| Hispanic Ethnicity, n (%) | <0.0001 | <0.0001 | |||||
| Non- | 234 (73%) | 420 (71%) | 2341 (86%) | 151 (79%) | 1813 (93%) | ||
| Hispanic | |||||||
| Hispanic | 87 (27%) | 175 (29%) | 369 (14%) | 39 (21%) | 139 (7%) | ||
| Marital Status, n (%) | <0.0001 | <0.0001 | |||||
| Single | 141 (46%) | 281 (50%) | 588 (23%) | 41 (23%) | 153 (9%) | ||
| Married/partner | 123 (40%) | 194 (34%) | 1652 (65%) | 67 (37%) | 1069 (59%) | ||
| Divorced/separated/widowed | 45 (15%) | 90 (16%) | 288 (11%) | 72 (40%) | 578 (32%) | ||
Survival of patients (A) age 15-64 and (B) age 65+ by insurance status at diagnosis.
Survival of patients (A) age 15-64 and (B) age 65+ by insurance status at diagnosis.
Fathi:Seattle Genetics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda Pharmaceuticals International Co.: Research Funding; Ariad: Consultancy; Exelexis: Research Funding; Agios: Membership on an entity's Board of Directors or advisory committees; Merck: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal