In this issue of Blood, Hagner et al provide preclinical evidence that CC-122 might be active in both major molecular subtypes of diffuse large B-cell lymphoma (DLBCL).1
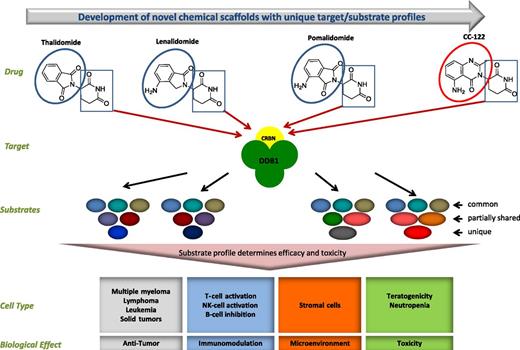
Schematic model of cereblon (CRBN) binding and differential substrates resulting in pleiotropic activity. The boxes outlined in blue represent the common glutarimide moiety responsible for CRBN binding, and the circle outlined in red highlights the structural difference from the phthalimide moiety. CC-122 shares the same molecular target, CRBN, as lenalidomide, pomalidomide, and thalidomide; however, differential substrate profiles and/or kinetics of substrate degradation can manifest different biological effects that are cell-type dependent. DDB1, DNA damage-binding protein 1; NK, natural killer. Figure courtesy of Celgene Corporation.
Schematic model of cereblon (CRBN) binding and differential substrates resulting in pleiotropic activity. The boxes outlined in blue represent the common glutarimide moiety responsible for CRBN binding, and the circle outlined in red highlights the structural difference from the phthalimide moiety. CC-122 shares the same molecular target, CRBN, as lenalidomide, pomalidomide, and thalidomide; however, differential substrate profiles and/or kinetics of substrate degradation can manifest different biological effects that are cell-type dependent. DDB1, DNA damage-binding protein 1; NK, natural killer. Figure courtesy of Celgene Corporation.
The development and evolution of immunomodulatory drugs (IMiDs) is one of the most fascinating drug development stories in cancer medicine.2 This history began with their use as an antiemetic drug used in pregnancy and was abruptly halted because of the association with severe birth defects. Their testing in multiple myeloma was stimulated by their antiangiogenic effects and led to a new active class of drugs in multiple myeloma. Their utility in other hematologic malignancies continues to evolve with demonstrated activity in molecularly defined subtypes of DLBCL. After years of evolution driven by chemistry, preclinical work, and clinical experience, the next family member of the thalidomide analogs, CC-122, emerges with features that differentiate it from IMiDs, giving rise to a new class of drugs: pleiotropic pathway modifiers (PPMs; see figure). Novel properties make CC-122 potentially active in a subtype of DLBCL in which its predecessor, lenalidomide, has limited activity.
There are 2 subtypes of DLBCL: activated B-cell–like (ABC) and germinal center B-cell–like (GCB) subtypes.3 The former is characterized by tonic B-cell receptor (BCR) signaling and a significantly worse clinical outcome. Recognition of molecular subtypes of DLBCL, because of their different biology and pathogenesis, play an important role in the selection of therapy.4 Lenalidomide, as a single agent, demonstrates significant activity in relapsed and refractory DLBCL. However, the activity of lenalidomide alone or in combination with rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone (R-CHOP) appears to be confined primarily to ABC DLBCL.5,6 The activity of lenalidomide in ABC DLBCL has 2 postulated mechanisms: inhibition of the nuclear factor κB pathway downstream of BCR signaling and upregulation of the interferon death pathway.7 Although the first pathway is particularly important for ABC DLBCL because of tonic BCR/MYD88 signaling, the second effect appears to be able to potentially impact both GCB and ABC DLBCL. In this regard, Hagner et al demonstrated that in contrast to the IMiD lenalidomide, the PPM CC-122 has significant activity in preclinical models of both GCB and ABC DLBCL. Similar to IMiDs, the PPM CC-122 also binds to CRBN, which in turn affects ubiquitination of Aiolos and Ikaros by the Cullin 4 RING E3 ubiquitin ligase complex, leading to their subsequent proteasomal degradation. The studies of DLBCL tumor tissue from patients exposed to CC-122 from the ongoing clinical trial are particularly revealing and confirm that this in vitro mechanism occurs in the clinic. In turn, degradation of Aiolos and Ikaros leads to a direct antitumor effect mediated through the interferon pathway.
Important questions remain. First, this mechanism does not address why the IMiDs and PPMs have a different impact on GCB DLBCL despite that both target CRBN. Hagner et al nicely outlined potential hypotheses behind this observation, including the role of different metabolites (see figure); however, further studies are needed. Second, as the name of class indicates, the effect of CC-122 is pleiotropic; hence, other potential mechanisms for its activity in DLBCL can, and likely do, exist. Furthermore, like their cousins, the PPMs also have immunomodulatory effects and impact the nonimmune environment as well. These effects are difficult to reproduce in preclinical models.
The demonstration of preclinical activity of the PPM CC-122 in GCB DLBCL is important. Although GCB DLBCL is associated with superior outcomes, ∼15% to 20% of the patients will develop disease relapse with 24 months postdiagnosis when treated with R-CHOP.8 Once relapsed, DLBCL has a poor outcome regardless of molecular subtype, with the majority of these patients dying of the disease.9 Approximately a quarter of relapsing GCB DLBCL patients (3% to 5% of all) have so called “double-hit” DLBCL, with translocations of myc and either a bcl-2 or bcl-6 translocation. This group of patients poses a particular urgent clinical need because of a very aggressive course and chemorefractoriness.
The work by Hagner et al provides a strong rationale for studying PPMs in both molecular subtypes of DLBCL. Ultimately, the future of the PPM class will depend on the evidence of clinical activity in these 2 DLBCL subtypes. Careful molecular analysis of patients with DLBCL receiving CC-122 may lead to the identification of novel biomarkers, possibly reaching beyond the ABC vs GCB classification, and the currently presented work provides an excellent foundation for these.
Conflict-of-interest disclosure: G.S.N. has received consulting fees from Morphosis and research funding from Celgene and Bayer.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal