Abstract

Background: Non-transfusion-dependent thalassemia (NTDT) is a genetic disorder most commonly including beta-thalassemia intermedia (Beta-TI), HbE/Beta thalassemia (HbE/Beta thalassemia), and hemoglobin H disease (HbH disease). NTDT patients can be at risk of iron overload due to increased intestinal iron absorption triggered by chronic anemia, ineffective erythropoiesis and, possibly, decreased serum hepcidin. Despite NTDT is popular in southern China, there is little data evaluating iron overload in Chinese patients. This study aimed at investigating the occurrence, prevalence and severity of iron overload in Chinese population with NTDT.
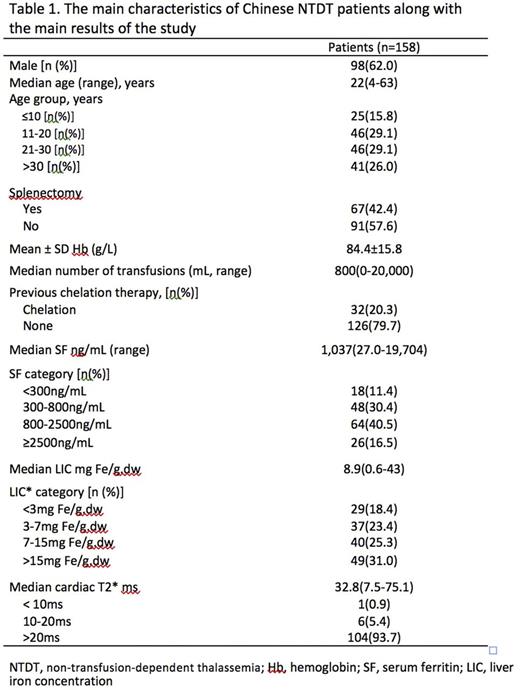
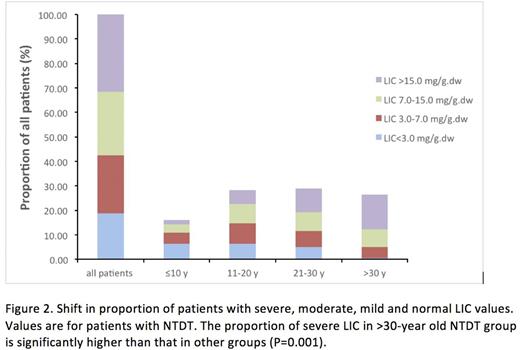
Methods: We evaluated the serum ferritin (SF), liver iron concentration (LIC) and cardiac T2* in 158 NTDT patients (83 with HbH disease, 45 with Beta-TI and 30 with HbE/Beta thalassemia) in China. The median age was 22 years old. The main characteristics of these patients along with the main results of the study were summarized in Table 1. Blood samples were obtained for the assessment of hemoglobin (Hb) and serum ferritin (SF) levels. LIC was assessed by using validated R2 magnetic resonance imaging [MRI] (FerriScan®). Cardiac iron level was measured by MRI T2*. Patients were scanned with MRI 1.5 T (Siemens Avanto, Germany). The study was performed at the First Affiliated Hospital of Guangxi Medical University. LIC < 3mg Fe/g dw and cardiac T2* > 20ms was considered normal. Abnormal LIC can be divided into mild: 3-7mg Fe/g dw, moderate: 7-15mg Fe/g dw, severe: >15mg Fe/g dw. All patients or parents/guardians provided their written informed consent to participate in this study. The study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University.
Results: The median SF level of 158 NTDT patients was 1,037(27.0-19,704) ng/ ml. LIC was detected in 155 patients (98.1%) and the median LIC value was 8.9(0.6-43) mg Fe/g dw. There were 15 patients (60%) (8 with HbH disease, 5 with Beta-TI and 2 with HbE/Beta thalassemia)<10 years old found liver iron overload. The youngest patient with liver iron overload was 5 years old with 5.6mg Fe/g dw in LIC. Cardiac T2*was assessed in 111 patients (70.2%) and the median cardiac T2* was 32.8(7.5-75.1)ms. The 7 patients (4.4%) (4 with HbH disease and 3 with Beta-TI) had cardiac T2*=<20ms. There was a significant correlation between LIC and SF (r=0.809, p<0.001). No correlation between LIC and Hb, cardiac T2* values can be verified.
There was a significant correlation between LIC and age (r=0.497, p<0.001)(Fig 1). The levels of LIC in patients > 30-year old group are significantly higher than those in other groups (Fig 2).The patients with Beta-TI and HbE/Beta thalassemia showed a statistically significant lower Hb and higher values of SF and LIC than those of HbH disease patients.
Conclusions: Chinese NTDT patients have a high prevalence of iron overload. The iron overload in patients with Beta-TI and HbE/Beta thalassemia are more serious than those in HbH disease patients. The age of patient is a risk factor of iron overload in NTDT patient. Patients > 30 years old have a high burden of iron overload. Our data shows that the first assessment of MRI LIC should be performed as early as 5 years old.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal