Abstract
HU is a myelosuppressive drug marketed since 1968 for the treatment of hematological malignancies, and authorized since 2007 in Europe as an orphan medicinal product for the prevention of recurrent vaso-occlusive crises and acute chest syndrome in adults and children older than 2 years with sickle cell disease (SCD). ESCORT-HU (European Sickle Cell Disease Cohort - Hydroxyurea) is a multicenter prospective non interventional study implemented in Europe to collect more information about the safety profile and morbidity-mortality in SCD patients treated with HU. The study responds to an EMA (European Medicines Agency) request and has been approved by the Ethical Committee of Necker Enfants Malades Hospital (Paris, France).
Some teratogenic effects of HU have been observed in fetuses of treated pregnant rodents (Woo, Katayama et al. 2004;Yan and Hales 2005 ;Chahoud and Paumgartten 2009). Hydroxyurea has been demonstrated to be embryotoxic at doses over 150 mg/kg/day in rats and in monkeys (Liebelt, Balk et al. 2007). Embryotoxicity was characterized by decreased fetal viability, reduced live litter sizes, and developmental delays. On the other hand, a recent study on pregnant mice showed no evidence of teratogenic effects with intraperitoneal injection of HU (25mg/kg) on gestation day (GD) 7.5 (Zhen Guan et al. 2015).
Due to the potential teratogenic effects in animal models, although no malformations have been reported in humans to date (Khushnooma et al. 2010,), the use of HU is not recommended during pregnancy.
The pregnancy in SCD can be associated with adverse maternal and perinatal outcomes. The rate of spontaneous abortion is more than 30% in our cohort at Necker Hospital and in literature (Regina Amelia Lopes Pessoa Aguiar et al. 2014, Sophie Lanzkron et al. 2012). Women of childbearing potential receiving HU should be advised to use contraception to avoid becoming pregnant. If there is a desire for pregnancy, HU must be stopped 3 to 6 months before conception and switched for chronic transfusion until the delivery or the end of breast feeding with a significant risk of allo-immunization (Ngo et al. 2010, Howard et al. 1995). In our experience, we have noticed that as pregnancies started frequently under HU, it is necessary to improve our knowledge about the use of HU during pre-conception or organogenesis in SCD patients and eventually develop new therapeutic strategies.
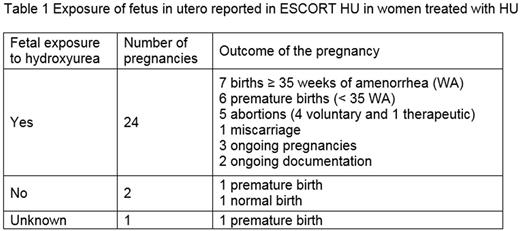
From June 2008 to July 2016, 1050 patients (496 children and 554 adults) were enrolled in ESCORT-HU from 3 European countries, Greece (11.7%), Germany (13.4%), and France (74.9%). Among the 315 women with childbearing potential (aged more than 15 to 49 years), 28 pregnancies in 27 women treated with HU have been reported despite the information to stop HU before conception (Table 1). Clinical data regarding the newborn are reported for 7 pregnancies with HU exposure and no malformations were observed.
In women treated with HU:
• HU was stopped in 15 (15 pregnancies) women during the first trimester of pregnancy (9 before 6 WA). The outcome of these pregnancies were 5 normal births, 5 premature births, 3 ongoing pregnancies, 1 voluntary abortion, 1 unknown
• HU was used during the whole pregnancy in 1 woman (issue normal birth),
• Information on treatment discontinuation was not reported in the database for 8 women.
In our study, a large majority of pregnancies (89%) occurred while HU was not stopped which correlates with the high rates of unplanned pregnancy in SCD women (Smith-Withley et al 2014, Eissa et al 2014). The use of HU during organogenesis or pre-conception period in our cohort seems to have no impact on the materno-fetal and new-born morbi-mortality which is consistent with literature data (Khushnooma et al. 2010).
Even if women of childbearing potential receiving HU should be advised to avoid becoming pregnant, in this series nested in the ESCORT HU cohort pregnancies occurred safely despite HU. These results are important because they could help to limit the indications and duration of transfusion and therefore the risk of allo-immunization and delayed hemolytic transfusion reaction in this at-risk population. Nevertheless this preliminary work needs to be confirmed by a comprehensive collection which could help us to evaluate the risk-benefit ratio, of HU versus blood transfusion during pregnancy in SCD women.
Ribeil:Bluebirdbio: Consultancy; Addmedica: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal