Abstract
Background
B-cell depletion with rituximab (RTX) is widely accepted as first- or second-line therapy in primary immune thrombocytopenia (ITP), but it is still unclear how RTX mediates its positive effect in ITP patients. RTX has been reported to induce a reduced titer of platelet antibodies. However, this finding is inconsistent and other B-cell functions, such as the ability to secrete cytokines or to function as antigen-presenting cells for T cells, may be involved in the pathogenesis of ITP. Evidence suggests that B cells participate in the regulation of autoimmune diseases by virtue of their ability to produce the regulatory cytokines interleukin (IL)-10, IL-35, or transforming growth factor β. The various functions of B cells involved in the pathogenesis of autoimmune diseases can in part be deducted by their phenotype as recognized by measurement of specific surface markers and cytokine secretion.
Materials and Methods
We previously conducted a trial involving 137 newly diagnosed adult ITP patients randomized to treatment with RTX (375 mg/m2/week for 4 weeks) + dexamethasone (DXM) (40 mg/day for 4 days repeated up to 6 cycles) or DXM monotherapy. From this cohort, we identified 16 patients with available samples of peripheral blood mononuclear cells (PBMCs) at baseline and 12 months after treatment; 9 patients from the RTX+DXM group, 7 patients from the DXM group. Seven anonymous blood donors served as healthy controls.
PBMCs were incubated for 18 h at 37°C under 5% CO2 in RPMI-1640 containing 10% (v/v) serum from healthy blood group AB donors, either alone or stimulated with 10 µg/ml CpG oligodeoxynucleotides. Expression of the cell-surface markers CD5, CD27, CD25 and CD19, and intracellular content of IL-6 and IL-10 were measured by flow cytometry.
Results
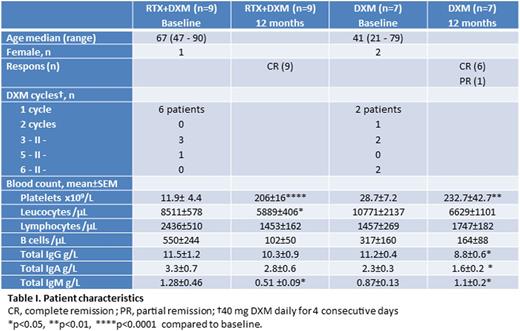
All patients responded to therapy and were in complete or partial remission at 12 months. Patient characteristics are listed in table I.
We observed a significant increase in the proportion of CD5+ B cells 12 months after treatment with RTX+DXM compared to baseline (p < 0.01, Fig. 1A). The percentage of CD27+ memory B cells was significantly decreased at 12 months compared to baseline in patients receiving RTX+DXM (p < 0.05, Fig. 1B), and there was an inverse correlation between platelet numbers and the proportion of CD27+ B cells (R = -0.71; p < 0.05). The proportion of CD25+ B cells tended to decrease in patients treated with RTX+DXM, and was lower at 12 months than in patients treated with DMX only (p < 0.05, Fig 1C).
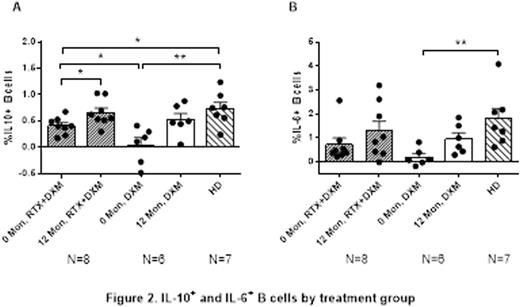
PBMCs from ITP patients contained a lower proportion of IL-10+ B cells (p < 0.01) as well as a lower proportion of B cells producing IL-6 (p < 0.01) at baseline than PBMCs from healthy controls. At 12 months the low proportions had normalized in both treatment groups (Fig. 2).
Conclusion
B cells from ITP patients treated with RTX+DXM contained a high proportion of CD5+ B cells and low proportions of CD25+ and CD27+ B cells. Before treatment, B cells from ITP patients contained low frequencies of IL-10+ and IL-6+ B cells. Treatment with RTX + DXM or DXM alone reverted these aberrancies to normal. The increase in IL-10+ B cells as well as CD5+ B cells, which may represent overlapping subsets, is compatible with induction of Bregs and may support Treg development. Given the role of CD5+ B cells in maintenance of tolerance, the high frequency of these cells, which has also been observed after RTX therapy in rheumatoid arthritis, is compatible with amelioration of disease.
Gudbrandsdottir:GSK: Research Funding; Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal