Abstract
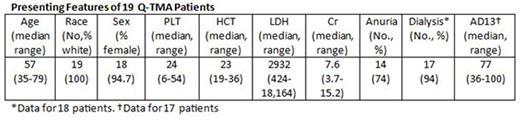
Q-TMA is an acute, severe, immune-mediated, drug-induced disorder. Q-TMA is suspected when symptoms suddenly begin within hours following quinine (Q) exposure. Diagnosis of Q-TMA is established by the history of recurrent acute symptoms following recurrent Q exposures and/or by documentation of Q-dependent antibodies reactive with platelets and/or neutrophils. The Oklahoma TTP-HUS Registry enrolls all patients for whom plasma exchange (PEX) is requested for suspected TTP or HUS. Since 1995, when routine measurement of ADAMTS13 activity began, the Registry has diagnosed 78 patients with acquired TTP (ADAMTS13 <10%). During this time we have also diagnosed 17 patients with Q-TMA; 2 additional patients were diagnosed before 1995. Seventeen of these 19 patients were tested for Q-dependent antibodies; all were positive. Nine patients had a history of recurrent acute symptoms with recurrent Q exposure, including the 2 patients not tested for Q-dependent antibodies. Q exposure was a pill in 18 patients, tonic water in one. Remarkably, 18 patients were women; all 19 patients were white. Common presenting symptoms were fever, chills, nausea and vomiting. No patients had focal neurologic abnormalities. All patients had microangiopathic hemolytic anemia (MAHA), thrombocytopenia, and acute kidney injury. Eight patients had elevated serum alanine aminotransferase (231-1345 U/L). Three patients had neutropenia (absolute neutrophil counts, 184-486). Two patients had coagulation abnormalities suggesting disseminated coagulation (DIC).
One patient died from complications of the central venous catheter insertion, performed for PEX and dialysis; all other patients recovered normal platelet counts. Three of the 18 surviving patients had end-stage renal disease (2 had kidney transplants). The median estimated glomerular filtration rate (GFR) for the other 15 patients, at 2.7-19.2 years (median, 10.2) after recovery, was 36 ml/min (range, 19-98). Only two patients had normal GFR (≥90 ml/min). Eleven patients had chronic kidney disease, defined by GFR <60 ml/min. Seven of 18 patients have died 4.1-12.7 years (median, 7.8) following recovery at ages 59-87 years. Conclusion. Quinine can cause severe immune-mediated toxicities involving multiple organ systems (Am J Hematol 2016; 91: 461). Q-TMA is an acute disorder causing severe kidney injury and, in some patients, also liver toxicity, neutropenia, and/or DIC. Q-TMA is not rare. During 20 years, we enrolled 17 Q-TMA patients compared to 78 patients with acquired TTP. Chronic kidney disease is a common long-term outcome. Explicit questions are required to discover the association of systemic symptoms with quinine ingestion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal