Abstract
Background: Ibrutinib, a potent irreversible inhibitor of Bruton's tyrosine kinase, is approved for the treatment of patients with mantle cell lymphoma (who have failed at least one prior therapy), chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL; including patients with 17p deletion), or Waldenström's macroglobulinemia. Ibrutinib exhibits pH-dependent solubility (insoluble at pH ≥ 3); therefore, pH-altering agents that increase gastric pH may have the potential to impact the pharmacokinetics (PK) of ibrutinib. Physiologically-based PK modeling and simulation suggested that an increase in gastric pH would minimally impact the bioavailability of ibrutinib. To evaluate potential drug interactions between ibrutinib and pH-altering agents, a phase 1 clinical study of the effect of omeprazole, a proton pump inhibitor (PPI), on the PK of ibrutinib in healthy adults was conducted.
Methods: An open-label, sequential-design drug interaction study of omeprazole coadministered with ibrutinib was conducted in healthy adults (18-55 years, inclusive). Key inclusion criteria included healthy men and women of non-childbearing potential, body mass index between 18 and 30 kg/m2, inclusive, and body weight ≥ 50 kg. On day 1, a single dose of ibrutinib (560 mg) was administered alone after an overnight fast. On days 3-6, omeprazole (40 mg) was administered alone 1 hr before breakfast. On day 7, omeprazole was administered after an overnight fast, and a single dose of ibrutinib was administered 2 hr after the omeprazole dose. Water was allowed ad libitum beginning 2 hr after ibrutinib dosing, and lunch was served ~4 hr after ibrutinib dosing.
Serial PK blood samples were collected over 48 hr following dosing on days 1 and 7. Key PK parameters for ibrutinib and its metabolite (PCI-45227) were summarized for each treatment. The effect of omeprazole was determined by assessing geometric mean ratios (GMRs) and 90% confidence intervals (CIs) for maximum concentration (Cmax) and area under the plasma drug concentration-time curve (AUC). Safety and tolerability were evaluated throughout the study.
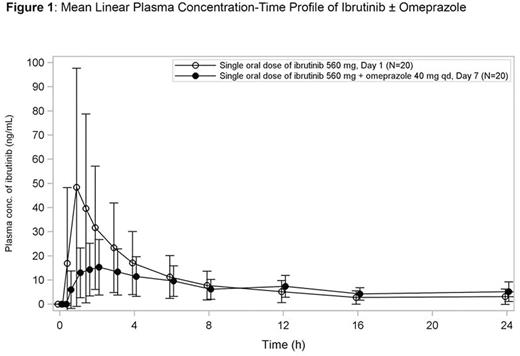
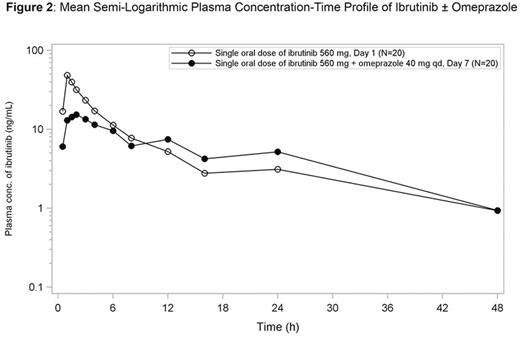
Results:Twenty healthy adults (95% men) completed the study; the median age was 48 yr and median body mass index was 25.8 kg/m2. The mean plasma concentration-time profile for ibrutinib is presented in Figures 1 and 2. AUC up to the last measurable concentration (AUClast) was similar for ibrutinib alone and in combination with omeprazole (GMR [90% CI] = 92.5%; [66.5 - 128.7]). Similar results were observed for AUC from time 0 to 48 hr (AUC48hr).
Cmax of ibrutinib alone was higher than that observed when ibrutinib was coadministered with omeprazole (39.5 vs. 14.8 ng/mL, respectively; GMR (90% CI) = 37.5% (25.1 - 56.0). Median time to maximum concentration (tmax) was longer with ibrutinib plus omeprazole (2.0 hr) than with ibrutinib alone (1.0 hr). A similar reduction in Cmax and delay in tmax was observed for PCI-45227; mean AUC of PCI-45227 was approximately 20% higher when ibrutinib was administered alone than when coadministered with omeprazole.
Whereas Cmax values were lower when ibrutinib was coadministered with omeprazole, the mean effect of omeprazole on AUC was minimal (<10%), albeit with a large CI. The AUC results were consistent with a population PK analysis which demonstrated that with the exception of a longer duration of absorption, coadministration of ibrutinib and antacids (mainly PPIs) under non-fasted conditions had no effect on PK parameters (Marostica E et al., Cancer Chemother Pharmacol 2015; 75:111-121). It should be noted that the effect of omeprazole coadministration on ibrutinib Cmax may be less pronounced under non-fasted conditions: because food intake itself increases gastric pH, dissolution and/or precipitation of ibrutinib in the stomach and intestinal tract would be similar for test and reference treatments.
The most commonly reported treatment-emergent adverse events (AEs) were back pain (3/20; 15%), headache (2/20; 10%), abdominal pain (2/20; 10%), and diarrhea (2/20; 10%), which were all grade 1 in severity. No serious AEs were reported.
Conclusions: Coadministration of omeprazole with ibrutinib decreased Cmax while marginally affecting AUC in healthy adults. Because AUC is deemed most relevant for ibrutinib's activity, coadministration of PPIs and other pH-altering agents with ibrutinib is not considered to have a clinically relevant effect on ibrutinib exposure.
de Jong:Janssen: Employment. Hellemans:Janssen: Employment, Equity Ownership. Jiao:Janssen: Employment. Sukbuntherng:Pharmacyclics, LLC: Employment, Equity Ownership; Global Blood Therapeutics: Equity Ownership. Ouellet:Janssen: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal