Abstract
Introduction
The nationwide TPOG-ALL-2002 protocol for treating children with acute lymphoblastic leukemia (ALL) was activated in January 2002 in Taiwan. To eliminate cranial radiation (CrRT)-related sequelae and minimize the adverse prognostic impact of traumatic lumbar puncture with blasts (TLP), we conducted a prospective study beginning in 1999 to modify CNS-directed therapy with delayed first triple intrathecal therapy (TIT) and omission of CrRT for all risk groups of newly diagnosed ALL. This approach improved CNS control at the single-institution study (J Clin Oncol, 2014) and has been used in whole TPOG since January 2009.
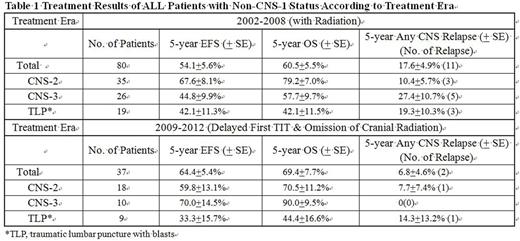
Patients with non-CNS-1 status (i.e., CNS-2, CNS-3 and TLP) have higher risk of CNS relapse and need intensive CNS therapy. On behalf of TPOG members, we reported the outcomes of these non-CNS-1 patients in the two eras (2002-2008 and 2009-2012) with or without the modified CNS therapy.
Methods
From 2002 to 2012, all newly diagnosed ALL children in Taiwan were enrolled in TPOG-ALL-2002 protocol (Leukemia, 2010). B-precursor ALLs were stratified into standard risk (SR), high risk (HR) and very high risk (VHR) groups, according to age, WBC count, cytogenetics and molecular analysis at diagnosis. T-cell ALL was designated as VHR. Since 2009, patients had been treated with TIT alone without CrRT. The first TIT was performed until the disappearance of blasts from peripheral blood (PB), no later than 10 days. SR patient with detectable PB blasts on day 8 was upgraded to HR group.
SR with CNS-1 received 14 doses of TIT, and those with CNS-2, or TLP got 2 additional TITs during induction and 3 additional TITs during maintenance therapy. Totally, SR with CNS-2 or TLP received 19 doses of TIT. And SR patients with CNS-3 or cranial nerve palsy at diagnosis were classified as HR. For HR with CNS-1, 17 doses of TIT were given. If HR groups with CNS-2, CNS-3, or TLP, they will receive total 25 doses of TIT including 2 additional ones during induction and 6 additional ones during maintenance therapy. Before 2009, only SR and HR with refractory CNS leukemia (failure to clear CSF blasts after 3 consecutive TITs) and those with CNS relapse will receive CNS radiation.
For VHR group before 2009, CrRT of 18 Gy was given to all patients at the end of remission induction. Instead, TIT was given for age < 2 years. After 2009, CrRT was totally omitted. VHR with CNS-1 received 19 doses of TIT. For VHR patients with CNS-2, CNS-3 or TLP at diagnosis, TIT was administered once/week until achieving CSF remission and then once 4 weeks during maintenance therapy.
Results
Since January 2009, all patients received TIT alone, irrespective of risk groups. The two cohorts, totally 1,366 patients, 909 treated with CrRT (2002-2008) and 457 without CrRT (2009-2012) were balanced in presenting features and distribution of CNS status. There were no significant differences between two eras in the event-free survival (EFS), overall survival (OS), incidences of isolated CNS relapse and any CNS relapse (Pediatr Blood Cancer, accepted June 2016).
The number of patients with CNS-2, CNS-3 and TLP were 35, 26 and 19 before 2009; and 18, 10 and 9 after 2009, respectively. Patients with younger age (< 1 year), higher WBC counts (> 100 X 109/L), HR/VHR or MLL rearrangement had significantly more non-CNS-1 status in the era of 2002-2008. And the significant factors prone to be non-CNS-1 were male, T-lineage and HR/VHR with the first TIT delaying. There were no significant differences between the two eras in the 5-year EFS and OS. Though the incidence of 5-year any CNS relapse was not significantly different, fewer relapses were observed in the era of 2002-2008 (Table 1). Before 2009, eleven CNS relapses experienced between 1 month and 3.1 years (median, 10 months) after remission. Two relapses after 2009 occurred on 1 month and 7 months, respectively.
Conclusions
Delayed first TIT until the clearance of circulating blasts and total omission of CrRT did not compromise the survivals and CNS control of childhood ALL patients with CNS-2, CNS-3 and traumatic lumbar puncture with blasts. Moreover, this approach prevents the adverse sequelae caused by CrRT. Furthermore, a skillful TIT is mandatory to improve results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal