Abstract
Background: We recently reported encouraging antileukemic activity of venetoclax, an orally available selective BCL-2 inhibitor, in combination with hypomethylating agents (HMA; NCT02203773) or low dose cytarabine (LDAC; NCT02287233) in patients aged ≥65 years with treatment-naive acute myeloid leukemia (AML) who are not fit for standard induction therapy [Pollyea et al, ASCO 2016 (abstract 7009); Lin et al, ASCO 2016 (abstract 7007)]. Here we present the genetic and molecular markers observed in this patient population, and their correlation with responses.
Methods: The data cut-off dates were: 10FEB2016 (venetoclax+HMA study), and 15FEB2016 (venetoclax+LDAC study). Patient responses were assessed according to the IWG criteria for AML.
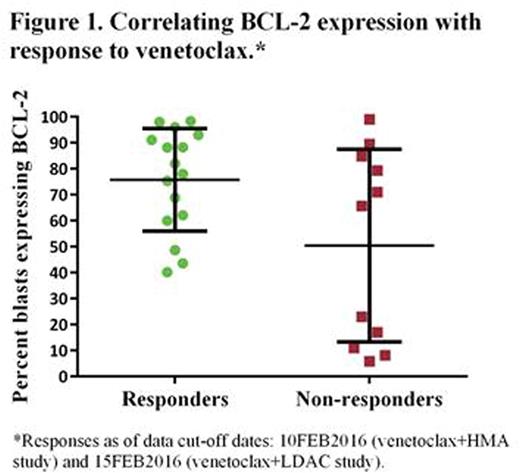
Given the selectivity of venetoclax to inhibit BCL-2, but not BCL-xL, the baseline expression of BCL-2 and BCL-xL proteins in blasts isolated from peripheral blood was determined by flow cytometry. The expression levels of BCL-2 were compared between those who achieved a response [complete remission (CR), CR with incomplete marrow recovery (CRi), partial remission (PR), morphologically leukemia free state (MLFS)] and those who did not achieve a response by the data cut-off dates [resistant disease (RD), progressive disease (PD)].
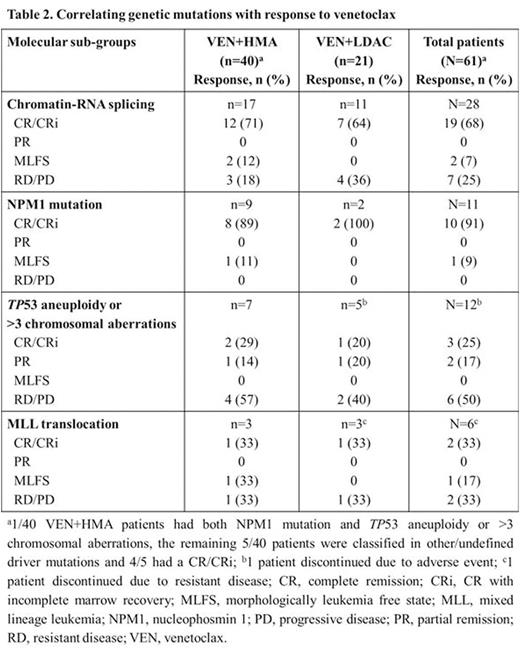
Next-generation sequencing (NGS) was performed on the blasts from bone marrow aspirates to identify recurrent mutations in genes associated with AML. Patients were classified into the following molecular subgroups based on the mutations data and site reported cytogenetics: (i) chromatin-RNA splicing group consisting of mutations in chromatin remodeling factors (ASXL1, EZH2), in splicing factors (SRSF2, SF3B1, ZRSR2), and/or in the transcription factor, RUNX1 (ii) NPM1 mutation (iii) MLL translocation (iv) TP53 mutations or >3 chromosomal aberrations (Papaemmanuil et al. NEJM 2016).
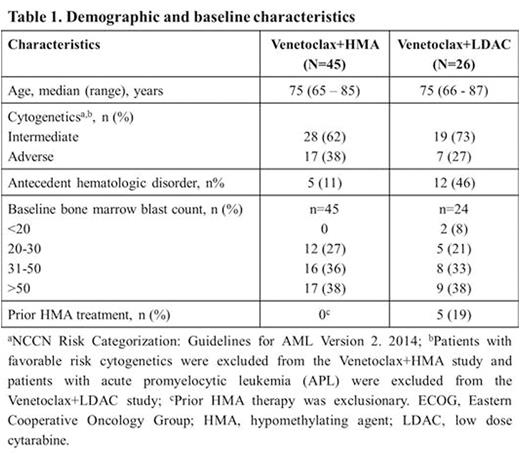
Results: Data from 45 patients enrolled in the venetoclax+HMA study and 26 patients enrolled in the venetoclax+LDAC study are reported here. The demographic and baseline characteristics are summarized in Table 1.
BCL-2 and BCL-xL protein expression were determined in 16/45 (36%) patients from the venetoclax+HMA study and 11/26 (42%) patients from the venetoclax+LDAC study. Remaining 44/71 (62%) patients were not included in this analysis for the following reasons: not evaluable for clinical response (n=7), non-availability of the specimen (n=8), and insufficient blasts in peripheral blood (n=29).
The percentage of blasts expressing BCL-xL was low (range 0-22%, median 0.6%), whereas the percentage of blasts expressing BCL-2 (BCL-2+) varied (6-99%, median 75%). 16/27 (59%) evaluable patients who achieved a response of CR/CRi/PR/MLFS had an average of 78% blasts BCL-2+. The remaining 11/27 (41%) patients who have not yet achieved a response had an average of 64% blasts BCL-2+ and were separated into two groups: a low percent of BCL-2+ blasts (median 11%, n=5) and a high percent of BCL-2+ blasts (median 82%, n=6) (Figure 1).
Pre-treatment bone marrow aspirates were available for NGS analysis from 40/45 patients (venetoclax+HMA study) and 21/26 patients (venetoclax+LDAC study). The data are summarized in Table 2. The chromatin-RNA splicing group comprised the largest subset of patients (n=28), of which 19 (68%) patients achieved a CR/CRi. Majority [10/11 (91%)] of the patients with NPM1 mutation had a CR/CRi. Conversely, 3/12 (25%) patients with TP53 aneuploidy or >3 chromosomal aberrations and 2/6 (33%) with MLL translocation achieved a CR/CRi to date.
IDH1/2 mutations were identified in 11/45 (24%) patients in the venetoclax+HMA trial and 7/21 (33%) patients in venetoclax+LDAC trial. 10/11 (91%) patients from the venetoclax+HMA trial and 5/7 (71%) patients from the venetoclax+LDAC trial were responders.
Conclusions: The results from this small data set showed that patients who achieved a response to venetoclax plus HMA or LDAC had a higher percent of blasts with BCL-2+. Among patients classified as non-responders, it remains to be determined if those with high percent of BCL-2+ blasts (n=6) will achieve a response with longer time on venetoclax therapy. Patients with specific genetic alterations such as chromatin-RNA splicing and NPM1 mutation may correlate with better odds of response to a venetoclax containing regimen. Samples are being analyzed to confirm these early findings as the two studies continue to enroll more patients.
Chyla:AbbVie Inc.: Employment, Other: may own stock. Popovic:AbbVie Inc.: Employment, Other: may own stock. Potluri:AbbVie Inc.: Employment, Other: may own stock. Hayslip:AbbVie Inc.: Employment, Other: May own stock. Huang:AbbVie Inc.: Employment, Other: may own stock. Zhu:AbbVie Inc.: Employment, Other: may own stock. Mabry:AbbVie Inc.: Employment, Other: May own stock. Bhathena:AbbVie Inc.: Employment, Other: may own stock.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal