Abstract
Introduction: Circulating fatty acids, which can serve as biomarkers of diet or activity of specific metabolic pathways, may influence non-Hodgkin lymphoma (NHL) risk by modulating inflammation or lymphocyte membrane stability. We performed prospective studies to evaluate red blood cell (RBC) membrane fatty acids as biomarkers of future NHL risk, hypothesizing a positive association for RBC saturated and trans fatty acids and an inverse association for polyunsaturated fatty acids (PUFAs) with risk of NHL and major NHL subtypes.
Methods: We conducted a nested case-control study among Nurses' Health Study (NHS) and Health Professionals Follow-up Study (HPFS) participants who provided blood samples in 1989-90 (NHS) or 1993-4 (HPFS). We confirmed 583 incident NHL cases through 2010 and matched one control per case on age, gender, race, and blood draw date. By gas chromatography we identified and determined membrane concentrations of 33 individual fatty acids in RBCs. We estimated the odds ratio (OR) and 95% confidence interval (CI) of NHL per 1 standard deviation (SD) increase in RBC level of specific fatty acids using unconditional logistic regression adjusted for matching factors. We also analyzed three common B-NHL subtypes individually (chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL), diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma) and examined all B-NHLs in aggregate with and without CLL/SLL.
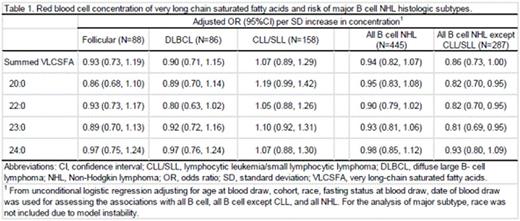
Results: We observed no associations between specific fatty acids and NHL risk overall (data not shown). In subtype-specific analyses, RBC very long chain saturated fatty acid (VLCSFA) levels (including the 20:0, 22:0, 23:0 fatty acids) were inversely associated with the group of all B-NHLs except CLL/SLL, with ORs suggesting 18% to 19% decreases in risk per SD increase in concentration (Table 1). We observed suggestive inverse associations of similar magnitude for follicular lymphoma and DLBCL but no clear association with CLL/SLL for these 3 VLCSFAs (Table 1). These three VLCSFAs had moderate to strong pairwise correlations; Spearman correlations were 0.61 for 20:0 with 22:0, 0.42 for 20:0 with 23:0 and 0.64 for 22:0 with 23:0. PUFAs were also inversely associated with all B-NHL except CLL/SLL, a finding primarily driven by RBC arachidonic acid levels [OR (95%CI) per SD: 0.83 (0.71, 0.90)] and suggestive also for follicular lymphoma [OR, 95% CI per SD: 0.79 (0.61, 1.02)] and DLBCL [OR, 95% CI per SD: 0.82 (0.64, 1.06)]. The remaining RBC fatty acids, including trans fatty acids, had no clear association with any NHL endpoint (data not shown). We did not observe heterogeneity by follow-up interval or age, although we had limited statistical power to detect significant heterogeneity for specific NHL subtypes.
Conclusion: RBC levels of VLCSFAs and PUFAs may be associated with lower risk of several types of B-NHL other than CLL/SLL. The specific fatty acids found to be related with NHL risk are not good biomarkers of diet, suggesting that the observed relations may instead be due to endogenous metabolic processes. Investigation is warranted into biologic mechanisms by which circulating fatty acids and their determinants may influence NHL risk, as is further examination of these associations in larger (ideally pooled) study populations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal