Abstract
Introduction
Midostaurin is an orally available multikinase inhibitor that blocks FLT3 kinase activity. FLT3 mutations are associated with more frequent and earlier relapses and worse survival. The phase 3 RATIFY trial showed that midostaurin compared with placebo improved overall and event-free survival in newly diagnosed pts with FLT3-mutated AML when administered in combination with standard chemotherapy and as single-agent maintenance (Stone et al, ASH 2015). The ongoing RADIUS trial (NCT01883362) is investigating whether adding midostaurin to SOC after alloHSCT reduces the risk of relapse in pts with FLT3-ITD-mutated AML. Here we report safety data from the first 56 enrolled pts.
Methods
RADIUS is a randomized, open-label, phase 2 study comparing SOC vs midostaurin + SOC after alloHSCT in adult pts with AML with FLT3-ITD mutations (planned enrollment, N = 60). Study treatment started 28-60 days after alloHSCT. SOC was dictated by the treating physician. Pts were randomized to either SOC or midostaurin 50 mg twice daily + SOC (hereafter called the midostaurin arm) continuously for ≤ 12 months and will be followed up for ≥ 24 months. The study was designed to look for any safety or efficacy signals and not powered to find differences between study treatments. The primary endpoint is relapse-free survival at 18 months after alloHSCT. Adverse events (AEs) were followed up for 30 days after treatment. Key inclusion criteria are documented FLT3-ITD mutation, age 18-70 years, and first complete remission status. Pts could enroll after the date of engraftment and hematologic recovery to an absolute neutrophil count > 1000/μL and platelet count ≥ 20,000/μL without requiring transfusion.
Results
Pts were randomized from Feb 5, 2014, to Jun 13, 2016. The 2 arms (n = 28 each) were balanced regarding age, sex, and race. Most pts (93%) had de novo AML. At data cutoff (Jun 3, 2016), data were not mature enough to evaluate efficacy. Median (range) follow-up in the SOC and midostaurin arms was 240 (3-786) and 234 (3-656) days, respectively.
Overall, 18 pts (64%) in the SOC arm and 19 pts (68%) in the midostaurin arm stopped treatment. Of these, 10 (36%) and 8 (29%) in the SOC and midostaurin arms, respectively, completed 12 months of treatment. Other reasons for stopping treatment were relapse (2 [7%] and 2 [7%]), death (2 [7%] and 0 [0%]), administrative problems (2 [7%] and 1 [4%]), withdrawn consent (1 [4%] and 3 [11%]), abnormal test results (1 [4%] and 0 [0%]), and AEs (0 [0%] and 4 [14%]).
In the 24 pts who received ≥ 1 dose in the midostaurin arm, the median midostaurin dose was 76.2 (range, 25-100) mg daily. In the 15 pts (54%) who required a dose change, the reasons for dose changes were AEs (13 [46%]), dosing error (3 [11%]), re-escalation (3 [11%]), abnormal test results (2 [7%]), per protocol (2 [7%]), use of concomitant strong CYP3A4 inhibitors (1 [4%]), and other reasons (4 [14%]).
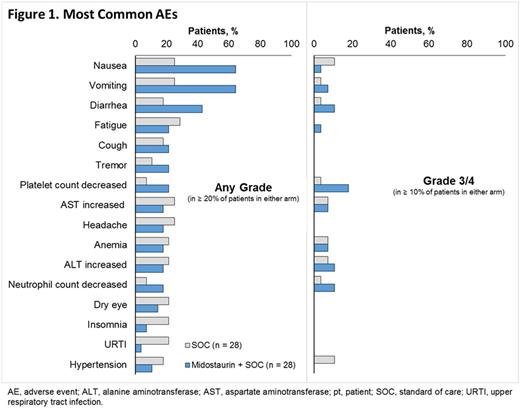
The most common any-grade (Gr) AEs were fatigue (29%) and AST, headache, nausea and vomiting (all 25%) in the SOC arm and nausea and vomiting (both 64%) and diarrhea (43%) in the midostaurin arm (Figure 1). The most common Gr 3/4 AEs were nausea and hypertension in the SOC arm (all 3 [11%] each) and diarrhea, increased ALT, neutrophil count decreased (all 3 [11%] each) and platelet count decreased (5 [18%]) in the midostaurin arm. No on-treatment deaths occurred in the midostaurin arm.
AEs led to discontinuation of midostaurin in 4 pts and included Gr 1 nausea, Gr 2 nausea and vomiting, Gr 3 lung infection, and Gr 2 elevated liver enzymes (n = 1 each). All of these except the lung infection were considered related to midostaurin.
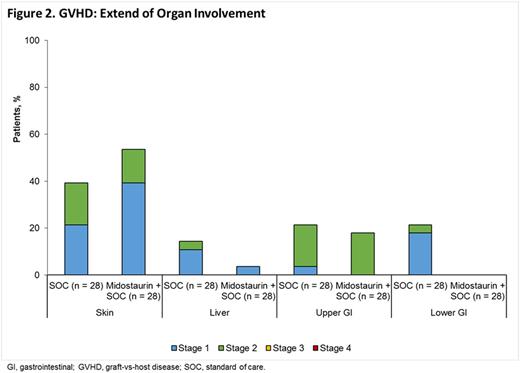
Graft-vs-host disease (GVHD) occurred in 16 pts (57%) in the SOC arm and 18 pts (64%) in the midostaurin arm (Figure 2). No stage ≥ 3 organ involvement occurred. Most cases of GVHD (11 [39%] in the SOC arm and 17 [61%] in the midostaurin arm) were acute. The most commonly affected organ was the skin (11 [39%] and 13 [46%], respectively, of which 5 [18%] and 4 [14%], respectively, were stage 2).
Conclusions
The preliminary safety data in the post-alloHSCT setting was consistent with data from other studies. Rates of Gr 1/2 nausea, vomiting, and diarrhea were higher in the midostaurin arm. Midostaurin did not change rates of GVHD. Because of the limited duration of follow-up, effects on chronic GVHD are unknown. Follow-up is ongoing, with efficacy data anticipated in 2017.
Maziarz:Athersys: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees; Novartis Pharmaceuticals Corporation: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding. Scott:Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Research Funding, Speakers Bureau; Alexion: Speakers Bureau; Agios: Membership on an entity's Board of Directors or advisory committees. Deol:Jazz Pharmaceuticals: Consultancy. Haines:Novartis: Employment. Bonifacio:Novartis: Employment. Rine:Novartis: Employment. Fernandez:Fate Pharmaceuticals: Honoraria; Chimerix: Honoraria; Sanofi: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal