Abstract
Background: Optimization of transplantation modalities (Graft versus host disease (GVHD) prophylaxis, conditioning regimens, high level HLA typing and supportive care) has improved overall survival (OS) of patients (pts) with idiopathic severe aplastic anemia (SAA) undergoing matched related (MRD) or 10/10 unrelated donor (MUD) allogeneic transplantation (HSCT). OS is nowadays of more than 80% and thus may not be sufficient anymore to accurately assess outcome. New composite endpoints including surrogate markers of quality of life, such as GVHD, may fit better our current practice.
GVHD and relapse free survival (GRFS) have recently been reported in the context of hematological malignancies, as a surrogate marker of quality of survival (Holtan et al. blood 2014). However, this end point was not evaluated in the setting of SAA, with no need of GVT effect, but more concern regarding engraftment. Thus, we adapted from Holtan et al. a composite GRFS with the aim to provide more accurate evaluation of outcome after HSCT for SAA.
Methods: We analyzed adult pts undergoing first HSCT for SAA from a MRD or 10/10 MUD between 2004 and 2013 (Clinical data obtained throughProMISe [Project Manager Internet Server], an internet-based system shared by SFGM-TC centers). Informed consent was obtained in accordance with the Declaration of Helsinki.
Relevant events for GRFS were death, graft failure/loss, grade 3 to 4 acute GVHD and severe chronic GVHD, according to which one occurred first. We analyzed GRFS according to donor type. Moreover, prediction by dynamiclandmarkingwas used for continual reassessment of GRFS within the next 2 years following subsequent landmark times from 0 to 3 years after HSCT.
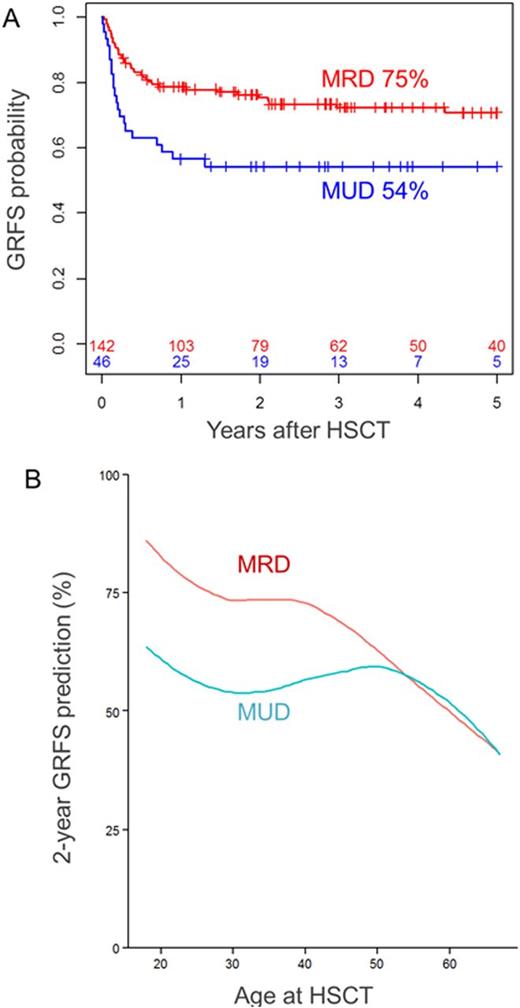
Results: 188 pts (MRD, n=142; MUD n=46) with a median age of 30 years (18-67) were analyzed. After a median follow-up of 52 months (3-159), 2-year GRFS were 75% and 54% in pts receiving MRD and MUD HSCT, respectively (p=0.006, Figure 1A). In Causes of GRFS failure in MRD vs. MUD were grade 3-4 acute GVHD (5% vs 20%, p=0.002), extensive chronic GVHD (3% vs 4%, p=0.902), graft failure/loss (10% vs 4%, p=0.236) and death before the previous events (7% vs 18%, p=0.057). The use of peripheral blood graft (PBSC) was associated with lower 2-GRFS compared to bone marrow (51% vs 74%, p=0.004).
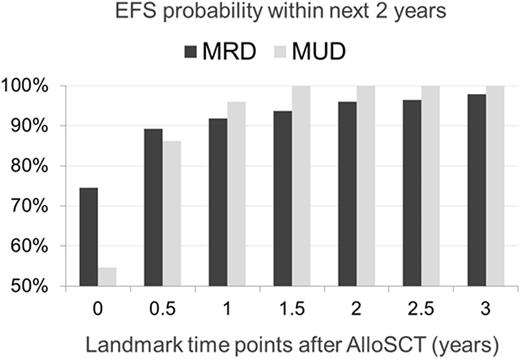
Multivariate Cox model showed that MUD (p<0.001), age (continuous variable, p=0.001) were associated with worse GRFS, with a significant interaction between these both variables (interaction p-value: 0.008, Figure 1B). PBSC as graft source (p=0.096) and positive donor and/or recipient CMVsero-status (p=0.095) tended to decrease GRFS. Although the pts in the MUD group initially have worse overall GRFS, prediction by dynamiclandmarkingshowed that after 6 months post HSCT, they recovered the same GRFS as those transplanted with MRD. Indeed, the probabilities to stay event-free within 2 years following the 6-month landmark time was 89% and 86% in the MRD and MUD groups, respectively (Figure 2).
Conclusion: GRFS after MRD HSCT is very good, with 75% of pts who did not present any events, supporting upfront HSCT for young patients with available MRD. In contrast, the higher incidence of acute GVHD (20% vs. 5%) after MUD significantly decreased GRFS compared to MRD. However, MUD pts surviving the early 6 months without may reach similar GRFS than pts transplanted with MRD. Taken together, these results suggest that although overall GRFS is good with low incidence of late events, early events such as acute GVHD remains a major cause of GRFS failure. This supports that the early post HSCT period remains a critical phase for the future good quality survival, underlining the importance of graft source choice as well as the need of GVHD prophylaxis improvement.
Peffault de Latour:Amgen: Research Funding; Alexion: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal