Abstract
Background: On the basis of the characteristics of extranodal natural killer T (NK/T)-cell lymphoma (ENKTL) which is predisposed to have the multidrug resistance phenotype and radiosensitivity, combined chemotherapy-radiotherapy is one of the effective options in localized early-stage, ENKTL, nasal type. However, frequent severe myelosuppression (grad 3/4 cytopenia), grade 3 radiation-related mucositis, and local/systemic relapse is a major obstacle. So we evaluated the proMACE-cytaBOM (prednisone, methotrexate, doxorubicin, cyclophosphamide, etoposide, cytarabine, bleomycin, vincristine, and methotrexate) as a slightly less intense regimen with sandwiched radiotherapy (36 Gy).
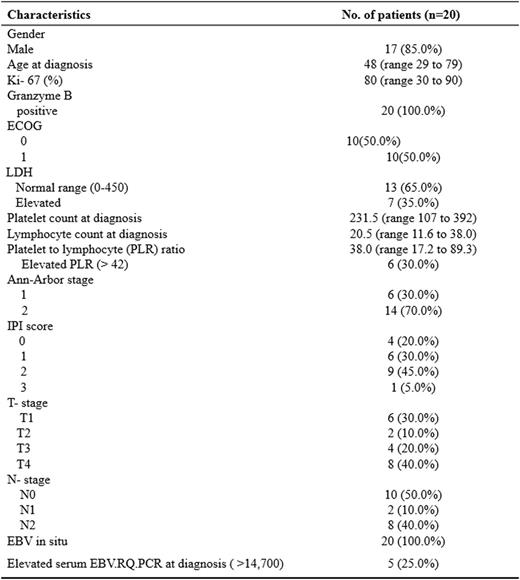
Patients and Methods: From July 2005 to December 2014, Thirty-one patients with newly diagnosed, stage IE to IIE, nasal type ENKTL were analyzed retrospectively. Twenty patients received the chemoradiotherapy sandwiched method: Initially 3 cycles of proMACE-cytaBOM, followed by radiotherapy of 36 Gy, after sandwiched radiotherapy and additional 3 cycles of proMACE-cytaBOM were administered. The other eleven patients were treated with following: Two patients received the frontline autologous hematopoietic stem cell transplantation, five patients were treated with sequential chemoradiotherapy as VIPD (etoposide, ifosfamide, cisplatin, and dexamethasone) followed by radiation of 50 Gy. Four patients received the chemotherapy alone (4 to 6 cycles of proMACE-cytaBOM).
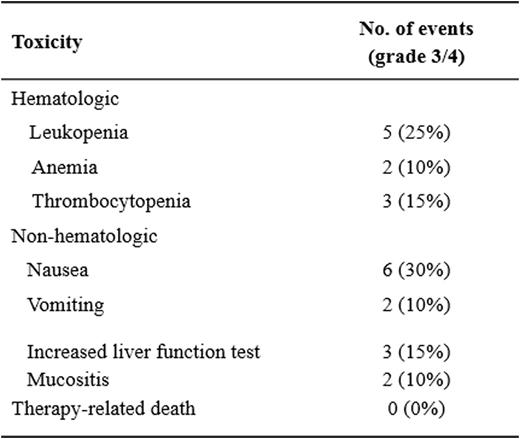
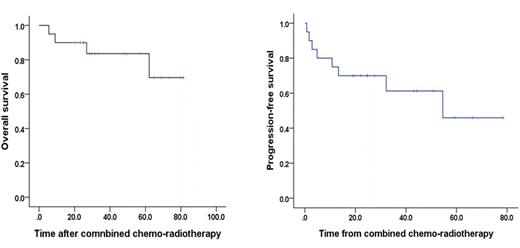
Results: In twenty patients with completely proMACE-cytaBOM and sandwiched radiotherapy schedule, median age was 50-year (range 26 to 79), with male-dominant (85%). A median of 6 (range, 4-6) cycles of proMACE-cytaBOM were administered, and sandwiched radiotherapy was received with a median 36 Gy (range 34.5 to 36) (Table1). Interim analysis after 3 courses of proMACE-cytaBOM showed that an overall response rate (ORR) of 82.6%, with complete remission (CR) and partial remission (PR) achieved in 73.9% and 8.7%, respectively. On treatment completion with chemotherapy and sandwiched radiotherapy, the ORR was increased to 90.0%, with CR rate increased to 85%. One patient experienced disease progression, and the other one was within stable disease during therapy. With a median follow-up of 42 months (range 5.5 to 81.4), the 5-year overall survival and progression-free survival were 83.6% (95% CI, 69 to 95 %) and 45.9% (95% CI, 45 to 95%), respectively (figure 1). Grade 3/4 neutropenia developed in 25% (n=5) of patients and grade 3 radiation-related mucositis in 10% (n=2). There was no regimen treatment-related mortality (TRM) (Table 2).
Conclusion: The proMACE-cytaBOM regimen with sandwiched radiotherapy (36 Gy) could be a promising and feasible option in the treatment of newly diagnosed localized ENKTL due to its favorable efficacy and tolerable low toxicities including of low radiation-related mucositis and no TRM.
major adverse events of therapy in twenty patients with localized ENKTL
Overall survival and progression-free survival after combined chemotherapy with sandwiched radiotherpay
Overall survival and progression-free survival after combined chemotherapy with sandwiched radiotherpay
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal