Abstract
Multiple myeloma (MM) is characterized by clonal proliferation of transformed plasma cells1 and is extremely dependent on bone marrow (BM) niche molecules and cells, such as osteoclasts. Unlike osteoclasts, the roles of BM adipocytes (BMAs) in MM are poorly understood, despite their great therapeutic potential. This year we published a study of body composition PET/CT parameters that serve as predictors of monoclonal gammopathy of undetermined significance (MGUS) progression to MM(Veld J, O'Donnell EK, Reagan MR, et al. Abdominal adipose tissue in MGUS and multiple myeloma. Skeletal Radiol.). We found that recently diagnosed MM patients had higher abdominal white adipose tissue (WAT) than MGUS patients, even after correction for BMI. Bone Marrow Adipose Tissue (BMAT), a newly appreciated adipose depot with endocrine and paracrine signaling functions, resides near MM cells and has unique expression profiles and phenotypic responses compared to WAT. Because obesity and aging, risk factors for MM, correlate with increased BMAT, and BMAs and MM cells are closely physically associated, we hypothesized that BMAs contribute to an optimal microenvironment for MM cell proliferation and/or drug resistance.
We performed direct and indirect co-culture experiments to study the effects of BMAT and BMAT-derived cytokines and lipids on MM proliferation and chemoresistance. MM cells were cultured on, or with conditioned media (CM) from, human and mouse BM-derived mesenchymal stem cells (MSCs) differentiated into adipocytes. MM proliferation, assessed by bioluminescence imaging, was dependent on MM cell line, MSC donor, and adipogenic stage.
IL6 is a highly potent MM-supportive cytokine elevated in MM patient BM and thought to be derived mainly from MSCs. MM cells (OPM2 and MM1R) grown in CM from MSCs differentiated for 21 days into adipocytes (Fat CM) treated with IL6 neutralizing antibodies had significantly decreased proliferation vs MM cells treated with Fat CM alone. MM1S cells also showed this trend. These data identified BMAs as a novel BM IL6 source. MM cells typically proliferated in response to donor "lipid fractions", the oil layer on top of human hip surgery BM samples, after 24, 48 and 72 hours, although donor variability was again observed. Lipid droplet content (Oil Red O quantification) of these BMAs also significantly decreased upon culture with MM cells, suggesting that MM cells induce lipolysis or uptake BMAT lipids to fuel their proliferation.
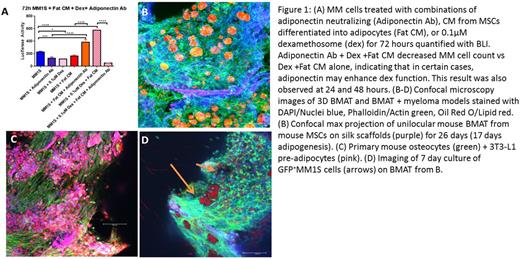
In contrast to the literature, we found that adiponectin can be either MM-supportive or MM-inhibitory, depending on the MM line tested and on the presence of dex. Certain MM cell lines (MM1S) became dexamethasone (dex) resistant when treated with Fat CM. Strikingly, all 3 cell lines tested (MM1S, MM1R and OPM2) showed significant decreases in cell number at 24, 48 and 72 hours after treatment with a neutralizing adiponectin antibody vs IgG control, when grown in the presence of 0.1μM dex + Fat CM (which contained high levels of adiponectin from ELISA analysis) (Fig 1A). These data suggest that adiponectin can induce dex resistance, indicating that adiponectin inhibitors + dex may be a novel MM therapy.
Lastly, we developed a physiologically relevant 3D in vitro tissue engineered BMAT model utilizing biocompatible, porous silk fibroin scaffolds to more accurately define BMA-MM interactions. Our 3D models provide the correct mechanical robustness and biomaterial properties to mimic trabecular bone and unilocular BMAT (Fig 1 B-D). We generated long-term cultures of BMAT from MSCs and cultured MM cells (GFP+ MM1S) on these for up to 1 week, demonstrating the development of the first 3D BMAT artificial culture system, with or without MM cells. We are now using this novel platform to more deeply explore the relationship between BMAT and MM cells.
In conclusion, BMAT likely plays a role in MM progression. 3D tissue engineered models of the BM milieu are a crucial link between 2D and in vivo models, maintaining the high-throughput capacity of 2D studies and the translational relevancy of in vivo models. Our data demonstrate important interactions between BMAT and MM cells, highlighting our need for further research into the roles of BM adipokines and adipocytes in MM pathogenesis and chemoresistance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal