Abstract
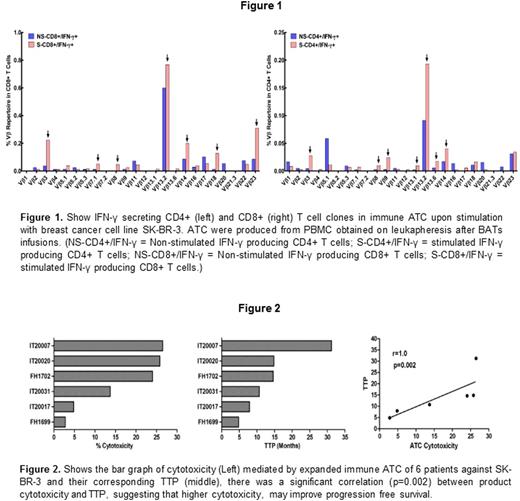
Background. In our recent phase I immunotherapy (IT) trial in 23 women with metastatic breast cancer (MBC), 8 infusions of activated T cells (ATC) armed with anti-CD3 x anti-HER2 bispecific antibody (HER2Bi) given in combination with interleukin-2 (IL-2) and granulocyte-macrophage colony stimulating factor (GM-CSF) induced specific anti-breast cancer immunity. This study investigated whether specific cellular and humoral anti-breast cancer immunity induced by infusions of HER2 bispecific antibody armed T cells (BATs) could be transferred after high dose chemotherapy (HDC) and stem cell transplant (SCT) in MBC patients. Methods. T cell were activated with OKT3 and expanded in IL-2. ATC were harvested, armed with HER2Bi, and cryopreserved in 8 doses for twice weekly infusions for 4 weeks along with IL-2 and GM-CSF. Seven to 14 days after the last infusion of BATs, the patient was leukapheresed again to obtain and expand immune T cells. Multiple infusions of immune ATC after the HDC and SCT were given to boost the transferred cellular and humoral immune responses which were monitored up to 24 months. Results. Six of 8 MBC patients enrolled were evaluable in the protocol, no dose-limiting toxicity, delays in engraftment, or life-threatening infections were observed. Five of 6 evaluable patients exhibited increased anti- breast cancer cytotoxicity and IFN-γ Elispots after vaccination with BATs and up to 18 months post SCT. Serum and culture supernatants from in vitro antibody synthesis assay showed gradual increases in anti-SK-BR-3 IgG levels after SCT. Serum cytokine profile showed increases in IL-12 and Th1 cytokines. One out of 6 evaluable patients who rapidly progressed showed poor immune response, had high serum levels of Th2 cytokines and no evidence of transfer of immunity. Flow cytometry analysis of Vβ repertoire pattern in PBMC collected post IT and post SCT indicate transfer of the major Vβ clones post SCT that produced IFN-γ upon stimulation with breast cancer cells (Fig. 1). A significant correlation (r=1.0; p<0.002) between immune ATC cytotoxicity directed at breast cancer cells and time to progression (TTP) suggests that more robust vaccinations with a Th1 shift in cytokine profiles can lead to clinical benefit (Fig. 2). Conclusions. Our pilot study suggests that cellular and humoral immunity was transferred and boosted using immune T cells after SCT. There was robust reconstitution of T and B cell functions early after SCT as evidenced by CTL and NK activity, IFN-γ EliSpots, in vivo/in vitro antibody synthesis, and Th1 cytokine responses.BATs induced endogenous anti- breast cancer cellular, humoral and innate immunity that could be detected after SCT and may have provided clinically meaningful anti-tumor immunity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal