Abstract
Introduction:
HL is highly curable, with overall survival (OS) rates of approximately 85-90%. A primary goal of treating patients is to optimize disease control while minimizing late effects. Compared to chemotherapy alone, combined modality therapy improves 1-3 year progression free survival by approximately 5% with equivalent OS rates. Cardiovascular late effects are the leading non-malignant cause of death among survivors; however, there remains considerable uncertainty regarding long-term cardiac risk from contemporary therapy. To help provide the framework for informed decisions, we conducted a systematic review to estimate cardiovascular late effects after HL treatment. We sought studies focused on patients who had received contemporary treatment regimens and on cardiac outcomes important to providers and patients.
Methods:
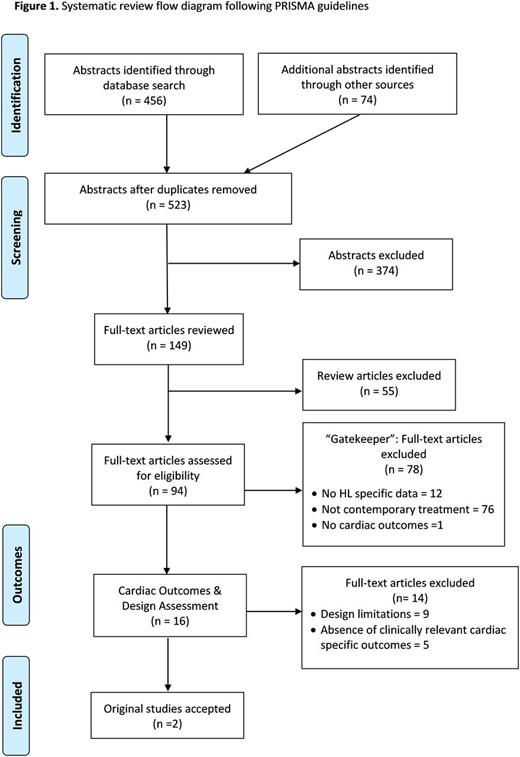
Our multidisciplinary study team, including pediatric and adult hematologists, a cardiologist, and decision experts, systematically reviewed the published literature. We searched MEDLINE/PubMed (from inception-December 30, 2015) and the Cochrane Database of Systematic Reviews (from 2005-December 30, 2015). Our search combined specific MeSH and text words using the following search groups: HL, cardiovascular outcomes, treatment related terms and cardiac outcome-specific terms.
We included only articles published after 1990 as the mid-1990s saw both a shift away from mantle radiation and the incorporation of anthracyclines. We also conducted a citation analysis of review articles. We included abstracts of studies of human subjects with HL if they reported cardiac toxicity after treatment. We excluded abstracts of studies published prior to 1990, with follow up < 5 years post initial treatment completion, with 10 or fewer subjects, studies of relapse treatment, studies for which full text was not in English, and letters and editorials.
For retained abstracts, we then performed a "gatekeeper" full text review to identify which studies reported information needed to estimate individual cardiac risk. We retained articles if (1) they reported HL-patient specific results, (2) at least half of the study's HL patients received their initial treatment during the "contemporary" era (post 1990); and (3) they reported cardiac outcomes. We then evaluated studies passing gatekeeper review to determine if (1) they reported clinically relevant cardiac outcomes; and (2) it was possible to calculate rates for outcomes of interest.
Results:
We identified 523 abstracts and excluded 374. Of the 149 remaining articles, we excluded 55 reviews, leaving 94 for full text review. We excluded 78 studies based on our gatekeeper criteria, leaving 16 articles. We excluded 14 of these 16 articles, in some cases for multiple reasons, including the absence of clinically relevant cardiac outcomes and design limitations making individual risk estimation not possible. Our initial systematic review therefore identified only 2 studies that satisfied all criteria1, 2.
Finally, we reassessed the 94 articles satisfying our abstract inclusion criteria. We found that although we could not estimate individual late effect cardiac risk following contemporary HL treatment from results for 92 of these studies, obtaining the primary data would likely make such estimation possible. We identified studies reporting relevant cardiac outcomes with approximately ≥ 100 HL patients who had received contemporary therapy.
Conclusion:
Our systematic review identified only 2 studies reporting results that could be used to estimate contemporary treatment cardiac late effects. Even papers published within the last 5 years often did not report separate results for patients receiving contemporary vs. early therapies. We are now seeking to obtain and pool patient data across international datasets to estimate risks for multiple cardiac outcomes. Risk assessment will help guide patient-centered discussions by predicting cardiovascular toxicity for HL patients treated with modern therapy.
References:
1. Aviles A, Neri N, Nambo M, et al. Late cardiac toxicity secondary to treatment in Hodgkin's disease. A study comparing doxorubicin, epirubicin and mitoxantrone in combined therapy. Leuk Lymphoma 2005; 46 (7): 1023-1028.
2. Galper SL, Yu JB, Mauch PM et al. Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation. Blood 2011;117(2):412-418.
Cohen:Joshua Cohen receives support from companies that develop and market medical therapies, some of which may relate to the subject of this abstract.: Consultancy. Evens:Takeda: Other: Advisory board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal