Abstract
Aims/Objective:Congenital antithrombin (AT) deficiency, estrogen-containing oral contraceptive pills (OCPs) and pregnancy are associated with increased risk of venous thromboembolism (VTE). Little is known about reproductive decision-making in women with AT deficiency. We sought to explore the attitudes and choices regarding reproductive health in this population.
Study Design/Methods:We conducted a provider-administered survey of women identified from the Mayo Clinic congenital AT deficiency database. Participants were asked to discuss their diagnosis of AT deficiency (age at diagnosis and VTE history including diagnosis and treatment) and questioned about (1) any lifetime methods of contraception, (2) pregnancies and pregnancy outcomes, (3) use of assisted reproductive technology, (4) history of menorrhagia, and (5) how their AT diagnosis had impacted each reproductive health experience and how this impact made them feel (open-ended question).
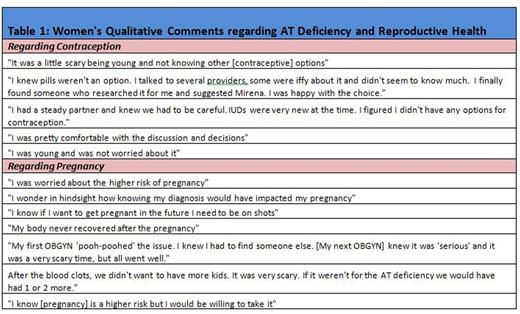
Results:Of 31 women with congenital AT deficiency, 18 (58%) were reached, 8 (26%) were not reachable and 5 (16%) were deceased. Of the 18 women who completed the survey, median age at AT deficiency diagnosis was 40 years (range 7 - 65). Twelve (67%) women had experienced a VTE; 2 and 5 women had VTE in the setting of pregnancy OCP use, respectively. Reported contraceptive methods included OCPs, intrauterine device (IUD), and male condoms. Of the 5 women diagnosed with AT deficiency while taking OCPs, three switched to IUD, one to condoms, and one did not report an alternative method of contraception. Fifteen (83% ) women reported at least one pregnancy (median number of pregnancies = 2; range 1 - 6). Of 42 total pregnancies among the 18 women, 33 (79%) resulted in live term birth, 3 (7%) in live preterm birth, and 6 (14%) in miscarriage/spontaneous abortion at a median of 12 weeks into the pregnancy. Four women (22%) reported the use of anticoagulation during pregnancy (presumed to be low molecular weight heparin, but most women could not specify), and 1 woman reported use of assisted reproductive technology leading to a successful pregnancy. Eleven women (61%) reported menorrhagia, 4 (36%) while on anticoagulation for VTE events. Ten of 18 women (56%) reported that the AT deficiency diagnosis had affected their reproductive health in at least one way. Patient-reported comments are presented in Table 1, and a "word cloud" diagram (an image composed of words from the women's comments regarding contraception), in which the size of each word indicates its frequency) is presented in Figure 1.
Conclusion:Women with AT deficiency require careful multidisciplinary management to avoid complications in the settings of hormonal contraception and pregnancy. Many women reported that their reproductive health experiences were impacted by their diagnosis, but also reported successful pregnancy outcomes. Validated questionnaires should be developed to assess women's reproductive health experiences. Strategies for reproductive risk management should be discussed carefully, and patient involvement in reproductive decision-making is key in this population.
Word Cloud depicting frequency of women's comments regarding AT deficiency and contraception
Word Cloud depicting frequency of women's comments regarding AT deficiency and contraception
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal