Abstract
Background: The myelodysplastic syndromes (MDS) are associated with shortened overall survival (OS) and inferior quality of life (QOL). Age, degree of comorbidity, MDS risk group, and treatment status are all likely predictors of both outcomes. We aimed to assess the association between treatment status and patient-reported QOL in a large cohort of community-treated MDS patients at the time of presentation to tertiary care, while controlling for the other three factors.
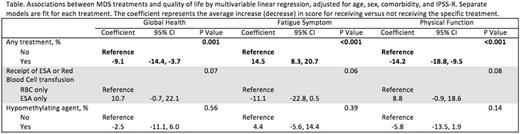
Methods: Beginning in 2006, patients with MDS presenting for their first evaluation at Dana-Farber Cancer Institute (DFCI) were enrolled into a clinical database (consent rate 85%). Enrollment included administration of the EORTC QLQ-C30 (Aaronson, JNCI, 1993), a 30-item measure of QOL that includes subscales for global health (higher score better), fatigue (lower score better), and physical function (higher score better). Medical record review was performed to characterize baseline demographic, clinical, and laboratory data. Treatment status included therapies received in the community during the 30 days prior to QOL assessment, as these were most likely to directly impact QOL. Comorbidity was assigned via the Modified Charlson Comorbidity Index (mCCI; Charlson, Journal Clinical Epi, 1994). MDS prognostic group was assigned via the IPSS-R (Greenberg, Blood, 2012). Associations between treatment status and QOL scores were analyzed with separate multivariable linear regressions adjusted for age, sex, comorbidity, and IPSS-R.
Results: In total, 287 patients with complete QLQ-C30 data were included, of which 22% were IPSS-R very high risk, 24% high risk, 22% intermediate risk, 26% low risk, and 6% very low risk. The majority of patients (66%) were male, median age was 68 years, and the mCCI was 0 in 40%, 1-2 in 35%, and 3+ in 24%. Relative to very low risk on the IPSS-R, the unadjusted hazard ratios for death were 1.5 for low risk, 2.2 for intermediate risk, 4.9 for high risk, and 7.2 for very high risk (Ptrend<0.001). In the 30 days prior to tertiary center evaluation, 52% of patients had received therapy: 40% red cell or platelet transfusions, 18% erythropoiesis-stimulating agents (ESAs), 11% either azacitidine or decitabine (HMA), 2.8% lenalidomide, and 2.8% deferasirox (treatments not mutually exclusive). Patients with higher risk disease on the IPSS-R were more likely to have received at least one treatment (41% for very low/low risk, 44% for intermediate risk, 57% for high risk, and 72% for very high risk; Ptrend<0.001). Associations between MDS therapies and QOL adjusted for age, sex, comorbidity, and IPSS-R are shown in the Table. Patients receiving any treatment in the 30 days prior to DFCI presentation experienced inferior global health and physical function, and increased fatigue in comparison to patients receiving no treatment. For patients with anemia, patients receiving an ESA without red cell transfusion experienced superior global health and physical functioning, and less fatigue compared to patients receiving transfusions (and no ESA). Patients receiving an HMA did not have significant differences in QOL compared to those who were not.
Conclusions: These data suggest that patients receiving MDS treatments have inferior QOL when compared to patients who are not treated, indicating a need for agents that better address the negative impact of MDS on QOL. Our results encourage the prospective study of the impact of different treatments, established and in development, on QOL. Our data also support the practice of an ESA trial before initiation of transfusions for MDS-related anemia, as the latter was associated with worse QOL even after adjustment for IPSS-R which includes degree of cytopenias. Finally, these results complement a recent report of minimal improvement in OS with HMA treatment in clinical practice (Zeiden, Leukemia and Lymphoma, 2016), suggesting that such treatment may also not be associated with significantly better QOL.
Steensma:Amgen: Consultancy; Genoptix: Consultancy; Celgene: Consultancy; Janssen: Consultancy; Millenium/Takeda: Consultancy; Ariad: Equity Ownership. Stone:Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy; Pfizer: Consultancy; Merck: Consultancy; Xenetic Biosciences: Consultancy; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy; ONO: Consultancy; Agios: Consultancy; Seattle Genetics: Consultancy; Celator: Consultancy; Jansen: Consultancy; Roche: Consultancy; Sunesis Pharmaceuticals: Consultancy; Karyopharm: Consultancy; Juno Therapeutics: Consultancy. DeAngelo:Novartis: Consultancy; Baxter: Consultancy; Celgene: Consultancy; Amgen: Consultancy; Pfizer: Consultancy; Incyte: Consultancy; Ariad: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal