Abstract
Mast cell (MC) activation syndrome (MCAS) is a recently recognized, heterogeneous disease of chronic multisystem inflammation (CMI) ± allergy. MCAS features aberrant MC reactivity and constitutive MC activation with little accumulation of MCs, distinct from mastocytosis [Afrin, Ann Med 48:190-201]. Whether clonality in MCAS is common is debated. Symptoms (sxs) range from mild to disabling, even life-threatening; prevalence may be as high as 17% [Molderings, PLoS One 8(9):e76241], underscoring the importance of studying MCAS. Notwithstanding case reports, small case series, and reviews to date, we report the first systematic characterization of a large MCAS cohort.
Methods: Under IRB-approved (Pro00015852, Pro00015857), Mastocytosis Society-sponsored protocols at one center, charts of 298 MCAS pts accrued retrospectively ("retro," diagnosed Nov 2008 - Sep 2012), plus 115 accrued prospectively (diagnosed Apr 2012 - Oct 2013), were reviewed for demographics, comorbidities (probs), sxs, family histories (FHs), physical exam and lab findings. For purposes of follow-up (f/u), data cut-off was June 30, 2014. Data were abstracted by LBA from available records. All were diagnosed with MCAS per criteria [Molderings, J Hematol Oncol 4:10] which in our experience (>1,000 pts) reflects MCAS behavior better than other proposals [e.g., Valent, Int Arch Allergy Immunol 157:215-25]. Blood samples from prospective pts were examined by flow cytometry for clonal MC disease (co-expressing CD45 and CD117 plus CD25 and/or CD2) and tested (ELISA kits, RayBioTech (Norcross, GA)) for elevated (↑) serum levels of cytokines (monocyte colony stimulating factor (M-CSF), granulocyte-macrophage colony stimulating factor (GM-CSF), interleukin-3 (IL-3), and tumor necrosis factor alpha (TNF-α)) potentially driving the mild relative monocytosis often seen in MCAS [Afrin, Blood 122:5240]; samples for cytokine testing were kept chilled from collection through assay, including centrifugation.
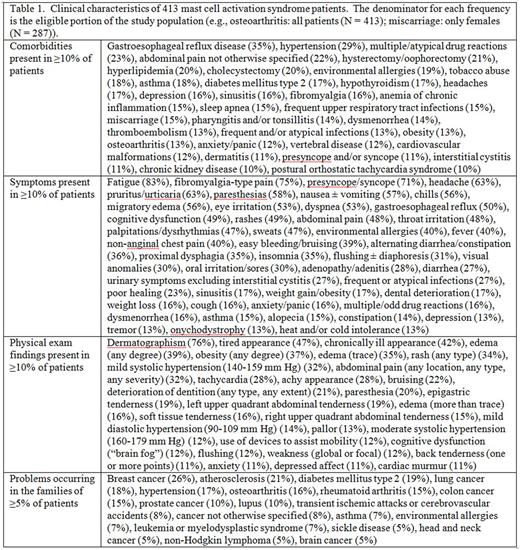
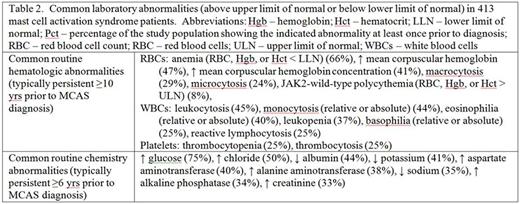
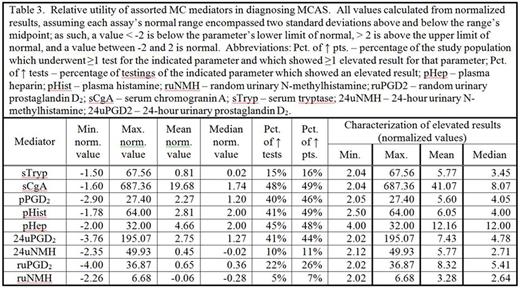
Results: Most of the 413 pts were female (69%) and Caucasian (75%). Median (med) ages at sx onset and diagnosis (dx) were 9 yrs (range 0-88) and 49 yrs (range 16-92). Med time from sx onset to dx was 30 years (range 1-85). Med number of probs was 11 (range 1-66). Med number of sxs was 20 (range 2-84). Med number of FH issues was 4 (range 0-33). Tables 1, 2, and 3 show pts' common clinical and lab characteristics and relative utility of various MC mediators in dx. Frequencies of clinical findings in our pts likely are underestimates due to retro assessment in 298/413 (72%). As reported before for the retro subset [Blood 122:5240], general laboratory abnormalities in these MCAS pts were common, modest, and persistent.
Most of our pts (72%) appeared chronically ill at times but overall healthier than expected from their many complaints, contributing to prior dx of somatism in most. Many pts "learned to live with it," no longer reporting some sxs unless asked.
In the prospective pts, flow cytometry failed to find the targeted signature of clonal MC disease. Serum M-CSF, GM-CSF, IL-3, and TNF-α levels were assessed and, despite correct negative and positive control results, were not found ↑ in any pt.
As of f/u cut-off, 388 pts (94%) were alive, 1 was lost to f/u and 24 pts (6%) had died of many causes (most commonly (25%) cancer). Data were insufficient to calculate meaningful survival statistics from time of dx.
Discussion: Long sx duration in MCAS - and cessation, of futility, in reporting sxs - show comprehensive history in pts with CMI is important. Routine lab abnormalities are seen long before dx but are modest and thus given short shrift by busy practitioners, but this study suggests they should spark thought of MCAS in pts with CMI and no unifying dx.
Relative utilities of MC mediators for dx in our pts were similar to a recent report [Zenker, Blood 126:5174] and further suggest serum tryptase - while still a good screen for MC neoplasia - poorly reflects MC activation.
Conclusions: MCAS is challenging to recognize, but its prevalence, morbidity, chronicity, and ability of most pts to identify helpful therapy merit attention to dx and treatment. Our data, characterizing MCAS more comprehensively than ever before, may facilitate its clinical recognition. More research is needed to identify etiologies (and linkages with chronic inflammatory diseases), facilitate dx, and guide therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal