Abstract
Introduction
Early detection of joint problems and musculoskeletal (MSK) abnormities is a priority in hemophilia care worldwide; however, there is no standard approach to screening. The World Haemophilia Federation Hemophilia Joint Health Score (HJHS) is well validated but requires time-intensive evaluation by a MSK expert (e.g. physical therapist, PT). Joint screening popularized for the US Center for Disease Control Universal Data Collection (UDC) focuses on range of motion (ROM) assessment only but is quick and easy to implement with modest staff training of non-experts. The approach used at our center, here dubbed UDC-plus, combines ROM measurements with pain and functional evaluation. In 2012 our center found that HJHS was sensitive but non-specific (high false positive rate) and correlated poorly with need for MSK referral or imaging [Morrison et al, Haemophilia, 18 suppl. 3 p.120]. The aim of this study was to evaluate the utility of using HJHS in clinical practice to predict need for MSK referral within 5 years of initial assessment. We also evaluated the ability of UDC-plus to predict actionable MSK findings at 5 years.
Methods
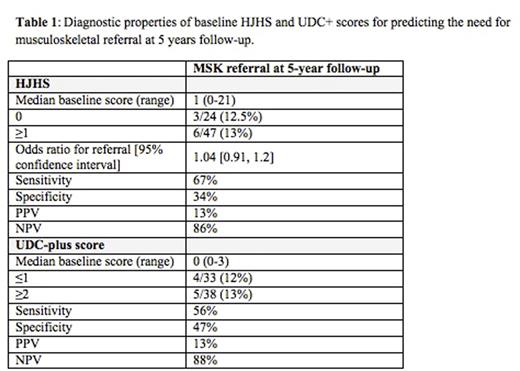
This is a single center, retrospective, observational study. Patients diagnosed with hemophilia A or B of any severity, a HJHS assessment between 2009 and 2011 and a PT evaluation 5 years later (between 2014-2016) during annual comprehensive visits at Boston Children's Hospital were eligible for the study. HJHS includes evaluation of 6 joints (elbows, knees, ankles) with score range from 0 to 124 points, considered positive if greater than 0. UDC-plus score includes the same joints with score range from 0 to 3, considered positive when 2 or greater. Outcomes included need for MSK-related referral during the 5-year observation period. Clinical and demographic characteristics were summarized using descriptive statistics; logistic regression was used to determine whether baseline joint scores were prognostic of referral. Sensitivity and specificity of joint scores were calculated.
Results
Seventy-one male patients met inclusion. Median observation time was 5.7 years (range: 3.2-6.8); median baseline age was 10.3y (3-21). Thirty-six (51%) had severe, 8 (11%) moderate and 27 (38%) mild hemophilia; 92% of severe and 25% of moderate patients were on regular prophylaxis. Nine (13%) patients had at least one TJ, reflecting that even for young patients in the prophylaxis era (after 1996 at our center), TJs are not eliminated. An abnormal score was found in 47 (66%) patients; only 6 (13%) of them required referral for PT, orthopedic or radiologic assessments. Of patients with abnormal baseline HJHS without initial MSK referral, 17/41 (42%) required at least one referral by 5 years while only 4/41 (10%) had an MSK concern at the 5-year comprehensive visit (other concerns were transient). Of patients with a normal baseline HJHS, 11/24 (46%) required at least one referral by 5 years and 3/24 (12.5%) required a referral at 5 years. Baseline HJHS was not prognostic of need for referral at 5 years, Table 1. An abnormal UDC-plus score occurred at baseline in 38 (54%) patients, 6 of whom (16%) received a referral. The sensitivity and specificity for the UDC-plus score were slightly less sensitive but more specific than HJHS.
Conclusion
While high sensitivity of HJHS makes it useful in a research setting, the time requirement by an expert PT and its poor correlation with need for either acute or long-term clinical intervention (low specificity) render it less desirable for screening in routine hemophilia care. UDC-plus, has modest sensitivity for acute and 5-year referral prediction, but is correspondingly more specific. Hemophilia comprehensive clinics require a basic joint assessment, which is neither time- nor resource-intensive. These data suggest HJHS does not meet this need; however, a more concise examination focusing on ROM of key joints, pain and functional status may be an important foundation. The UDC-plus with revised scoring criteria may support routine integration into hemophilia care without compromising clinic flow or costs.
Neufeld:Novartis: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal