Abstract

Background
U2AF1 mutations occur in approximately 16% of patients with primary myelofibrosis (PMF) and were significantly associated with anemia, thrombocytopenia, older age, JAK2V617F, ASXL1 mutations and normal karyotype (Leukemia 2014;28:431); furthermore, U2AF1 mutations were associated with inferior survival in univariate but not multivariable analysis. In the current study, we looked for the possibility of a differential effect from U2AF1 mutation variants on these observations in PMF.
Methods
Study patients fulfilled the 2016 WHO criteria for the diagnosis of PMF (Blood. 2016;127:2391). Additional selection criteria included the availability of U2AF1 mutational status. Previously published methods (Leukemia 2014;28:431), including targeted next generation sequencing (Blood 2015 126:354), were used to screen for U2AF1 and other prognostically-relevant mutations. Statistical analyses considered clinical and laboratory parameters obtained at time of initial referral to the Mayo Clinic.
Results
Patient characteristics:
U2AF1 mutational status was available for 457 patients and 72 (16%) harbored one of several mutation variants: these mutations affected residue Q157 in 44 (10%) patients, S34 in 24 (5%) and the remaining 1% displayed other variants. The 44 patients with U2AF1Q157 mutations included 23 with Q157P, 18 with Q157R and 3 with Q157-Y158insYE. The 24 patients with U2AF1S34 included 16 with S34F and 8 with S34Y. Only one patient harbored both Q157 and S34 mutations (Q157R, S34Y). Among all 457 study patients, median age was 63 years, 64% were males, dynamic international prognostic scoring system (DIPSS)-plus (JCO 2011;29:392) risk distributions were 13% low, 18% intermediate-1, 38% intermediate-2 and 32% high and driver mutation distributions were 54% JAK2, 22% CALR type 1/ type1-like, 4% CALR type 2/type 2-like, 7% MPL and 13% triple-negative. Cytogenetic studies were available in 449 patients: 39% abnormal and 10% unfavorable. All 457 patients were screened for ASXL1 mutations with 37% mutated, 450 for SRSF2 mutations with 15% mutated, 403 for SF3B1 with 8% mutated, 366 for IDH1/2 with 5% mutated and 369 for EZH2 with 4% mutated. Median follow-up was 4.4 years and during this period, 318 (70%) deaths and 53 (12%) leukemic transformations were documented.
Phenotypic correlates of U2AF1 mutation variants:
Because of the relatively small number of informative cases with specific mutations, we classified all patients into Q157 (n=44) and S34 (n=24) mutation variants and compared them with the 385 U2AF1 un-mutated cases. First, we confirmed our previous observations regarding the association between U2AF1 mutations in general and older age (p=0.0003), JAK2V617F (p<0.0001), ASXL1 mutations (p=0.0002), normal karyotype (p=0.03), hemoglobin <10 g/dL (p<0.0001) and platelet count <100 x 10(9)/L (p<0.0001); when the two U2AF1 mutation categories were analyzed separately, the corresponding p values for Q157 were 0.0005, 0.001, <0.0001, 0.04, <0.0001 and <0.0001 and for S34 were 0.12, 0.001, 0.41, 0.41, <0.0001 and 0.67.
Phenotypic correlates of U2AF1 mutation variants:
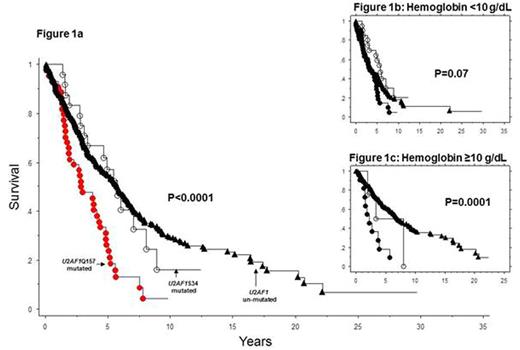
In univariate analysis, survival was adversely affected by U2AF1Q157 (p<0.0001; HR 2.2, 95% CI 1.6-3.1) but not by U2AF1S34 (p=0.8; HR 1.1, 95% CI 0.6-1.8) mutations (Figure 1a). Furthermore, the negative survival effect of U2AF1Q157 mutations was independent of anemia, thrombocytopenia, ASXL1, SRSF2, IDH1/2 and EZH2 mutations, as well as driver mutational status; multivariable analysis that included all molecular alterations identified U2AF1Q157 (HR 1.6, 95% CI 1.1-2.3), ASXL1 (HR 2.3, 95% CI 1.8-3.5), SRSF2 (HR 1.6, 95% CI 1.2-2.2) and absence of CALR type-1/like (HR 2.6, 95% CI 1.8-3.5) mutations as independent risk factors for survival. Finally, the survival effect of U2AF1Q157 mutations was independent of DIPSS-plus in patients with hemoglobin ≥10 g/dL (HR 2.6, 95% CI 1.3-5.3; p=0.007) (Figure 1c) but not in those with hemoglobin <10 g/dL (p=0.98) (Figure 1b).
Conclusion
Both U2AF1Q157 and U2AF1S34 mutation variants in PMF are associated with JAK2V617F and severe anemia whereas only the former is associated with ASXL1 mutations and thrombocytopenia. More importantly, U2AF1Q157, but not U2AF1S34, mutation variants in PMF are predictive of inferior survival, independent of other adverse mutations, and, in the absence of severe anemia, independent of DIPSS-plus.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal