Abstract
INTRODUCTION
Dermal fibrosis and sclerosis are pathologic features shared by Scleroderma-like chronic graft-versus-host disease (Scl-cGVHD) and Systemic Scleroderma (SSc). Moreover, in both diseases stimulating anti-PDGF-R antibodies were found, leading to abnormal collagen production by fibroblasts, eventually contributing to organ damage. Targeted therapy with tyrosine kinase inhibitors (TKI) like Imatinib and Nilotinib demonstrated clinical efficacy in Scl-cGVHD; however, the molecular basis underpinning the clinical effects are not fully elucidated. We investigated here a potential terapeutical target of the dermal cGVHD pathophysiology: the cellular and molecular features of pathological skin fibroblasts (GVHD-Fbs) and the efficacy of Nilotinib on fibrosis modulation.
MATERIALS AND METHODS
Fibroblast cultures (GVHD-Fbs) were obtained from skin biopsies of affected skin from 6 patients with active cGVHD, control fibroblasts are Human Dermal Fibroblasts adult (n-FBS).
Fibroblasts were characterized by flow cytometry (FACS CANTO II) for the detection of molecules: CD10, CD14, CD29, CD34, CD44, CD45, CD73, CD90, CD105, CD106, CD117, CD146.
In order to evaluate the adipogenic, osteogenic or chondrogenic differentiation cGVHD-Fbs and n-Fbs (n = 3) were cultured in differentiation medium (respectively NH AdipoDiff, NH OsteoDiff, NH ChondroDiff) after four passages. Intracellular lipid droplets indicated adipogenic lineage differentiation. The differentiation potential in the osteogenic lineage was evaluated by calcium accumulation, as assessed by Alizarin Red. The pellet obtained from chondrogenic lineage differentiation was embedded in paraffin, cut in the microtome and the sections placed on a glass slide were stained with Alcian Blue [Junker JP, Cells Tissues Organs, 2010].
For incubation with Nilotinib (Santa Cruz Biotechnology) the 10 mM stock solution was diluted to the final concentration in DMEM supplemented with 0,2% FBS (starvation), added to cell cultures at a concentration of 1 μM or 2 μM for 48h, which covered the mean plasma levels in cGVHD patients after standard doses.
In subsets of experiments, after starvation, fibroblasts were stimulated with recombinant TGFβ at 10 ng/ml (GIBCO, Invitrogen).
After incubation, total RNA was isolated and reverse transcribed. Gene expression was quantified by real-time PCR using the Sybr Green Mix for qPCR. Specific primer pairs for COL1α1 and COL1α2 were designed with the Primer 3 software. The transcript levels were normalized for the expression of GAPDH constitutive gene. Differences were calculated with the threshold cycle (Ct) and the comparative Ct method for relative quantification.
RESULTS
GVHD-Fbs are morphologically and phenotypically similar to normal fibroblasts (n-FBS).
GVHD-FBS did not show a different immunophenotype from n-Fbs, both in early and late culture passages. Also, no differences were noted between GVHD-Fbs and n-FBS in terms of multilineage differentiation capacity towards the adipogenic, osteogenic and chondrogenic lineage.
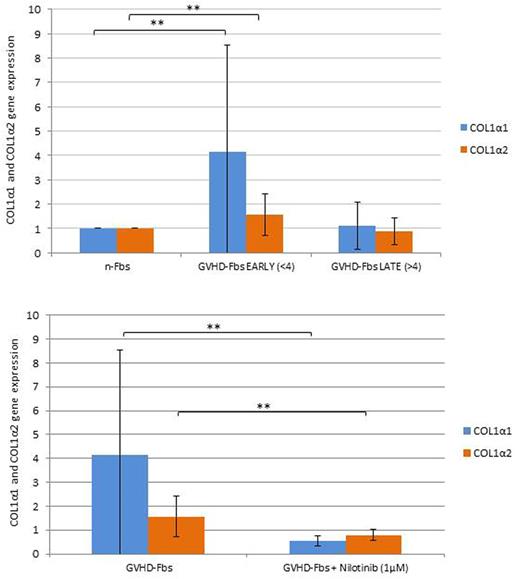
Gene expression of COL1α1 and COL1α2 in GVHD-Fbs was respectively 4 and 1,6 times higher compared to n-FBS (p = 0.02). However, the increased collagen expression was exclusive of early-passage GVHD-Fbs; in late-passage (>4) GVHD-Fbs, collagen mRNA levels were similar to n-FBS (p=0.6 for COL1α1; p=0.4 for COL1α2). As expected, TGFβ boosted collagen expression in n-FBS, but it did not increase COL1α1 and COL1α2 mRNA levels in GVHD-Fbs.
Therapeutic doses of Nilotinib (1μM) were able to reduce expression of COL1α1 and COL1α2 mRNA by 86,5% and 49%, respectively (p <0.01).
CONCLUSIONS
Early-passage GVHD-Fbs are a valuable cellular model to study the molecular mechanisms of cGVHD fibrosis in vitro, as they show increased collagen production, which is a strong hallmark of fibrosis. The failure to increase collagen expression in GVHD-Fbs upon TGFβ stimulation indirectly supports a TGFβ-dependent mechanism underpinning the fibrogenesis. Finally Nilotinib inhibits in vitro collagen expression in GVHD-Fbs confirming that the activity of TKI in Scl-cGVHD is mediated, at least in part, by direct antifibrotic effects on the fibroblasts.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal