Abstract
Introduction: Chemotherapy-induced FN is a clinically important adverse event that frequently requires hospitalization and can negatively impact treatment outcomes. Clinical guidelines recommend G-CSF primary prophylaxis when a patient's overall FN risk is >20%, so assessing individual FN risk is an essential step. Many newly discovered FN risk factors have been reported recently (eg, comorbidities such as diabetes, congestive heart failure,recent dermatologic conditions,and chronic obstructive pulmonary disease and procedures for cancer treatment). We sought to evaluate the added predictive value of these new risk factors beyond established FN risk factors.
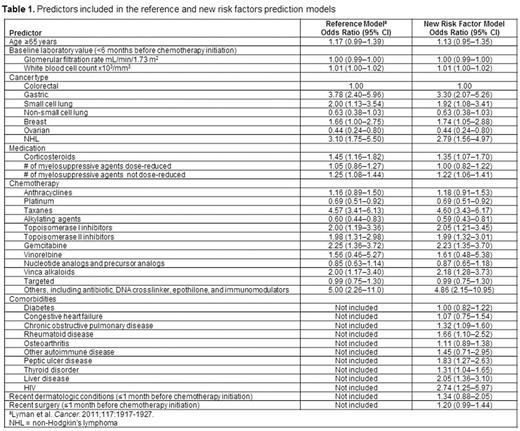
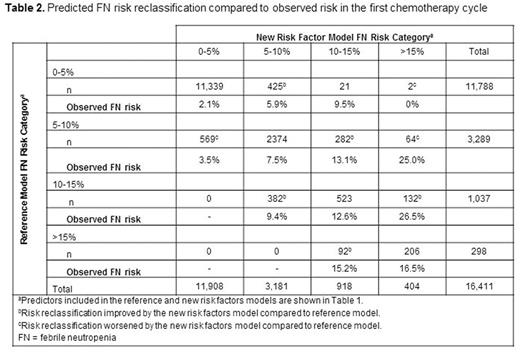
Methods: This study included patients diagnosed with lung, gastric, ovarian, colorectal, or female breast cancer or non-Hodgkin's lymphoma (NHL) at Kaiser Permanente Southern California (KPSC) between 2000 and 2009 and treated with chemotherapy. Patients who received prophylactic G-CSF or prophylactic antibiotics were excluded. Data were collected from KPSC's electronic medical records. The primary endpoint was FN in the first chemotherapy cycle. First, a reference model was developed based on a modified version of the FN prediction model published by Lyman et al (Cancer 2011;117:1917-27). Then a new prediction model based on the reference model plus additional newly identified FN risk factors was developed (predictors used in both models are shown in Table 1). Performance of the two models was evaluated by comparing their discriminative ability and calibration of predicted risk among the current study population. Discriminative ability was evaluated by examining the area under the receiver operator curve (AUC). Calibration of predicted risk was evaluated by comparing model-predicted risk to observed risk in the following FN risk ranges: 0-5%, 5-10%, 10-15%, and >15%. These ranges were chosen as approximately half of FN events occur in the first cycle; therefore, these ranges for FN risk in the first cycle are likely equivalent to 0-10%, 10-20%, 20-30%, and >30% risk over the chemotherapy course. Change in risk prediction at the individual patient level was also evaluated. For patients who developed FN, individual risk prediction was considered improved if the individual predicted risk drew closer to 100%; for patients who did not develop FN, individual predicted risk improved if it drew closer to 0%.
Results: A total of 16,411 patients were included in the analysis (36% breast, 23% lung, 20% colorectal, 3% gastric, 6% ovarian cancer, and 12% NHL). Mean age at diagnosis was 60.5 years. Most patients were Caucasian. FN incidence in the first chemotherapy cycle was 4.0%. The odds ratios for the predictors in both models are shown in Table 1. Comparison ofFN risk predicted by both models and observed FN risk are shown in Table 2. Addingnew risk factors did not result in significant improvement in discriminative ability: AUC changed from 0.72 to 0.73. However, adding new risk factors led to a more accurate risk classification for 12% of patients (n = 1946 [425 + 569 + 282 + 64 + 382 + 132 + 92]) while it led to a less accurate risk classification for only 0.01% of patients (n = 2, Table 2). Ofthe 701patients who developed FN in the first chemotherapy cycle, adding the new risk factors increased the predicted risk for 16% ofpatients (n = 115), but decreased the predicted risk for 10% ofpatients (n = 70). Of the 15,710patients who did not develop FN, adding the new risk factors decreased the predicted risk for 5.7% ofpatients (n =973) but increased the predicted risk for 5.2% of patients (n = 811).
Conclusions: Addition of the newly identified FN risk factors to the reference prediction model improved risk classification for FN in the first chemotherapy cycle. Since information on the new risk factors (including comorbidities such asdiabetes, congestive heart failure, chronic obstructive pulmonary disease, rheumatoid disease, osteoarthritis, other autoimmune diseases, peptic ulcer disease, thyroid disorder, liver disease, HIV,recent dermatologic conditions, and recent surgery)is readily available to clinicians, these factors could be incorporated into estimations of FN risk. Further refinement of the FN risk prediction model is warranted.
Li:Amgen: Employment, Equity Ownership. Family:Amgen: Research Funding. Chen:Amgen: Research Funding. Page:Amgen: Employment, Equity Ownership. Klippel:Amgen: Employment, Equity Ownership. Xu:Amgen: Research Funding. Chao:Amgen Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal