Abstract
Introduction:
HLH is an aggressive and life-threatening syndrome of excessive immune activation. HLH can be familial or secondary. Secondary HLH is usually associated with malignancy, infections or rheumatologic disorders. 27% of the secondary HLH are related to malignancy, the vast majority of which are hematologic malignancies (HM), and are associated with a mortality rate of 80%. Chemotherapy may not salvage these patients due to end-organ dysfunction at presentation (Johnson 2016). We sought to further describe the genetic landscape of HM associated HLH to identify potential targets for clinical trials.
Methods:
We queried the National Cancer Institute's Mitelman Database of Chromosome Aberrations and Gene Fusions in Cancer to identify patients (pts) with HM associated HLH. All identified references were reviewed and pt data was extracted regarding clinical and pathologic details as well as therapy and outcomes. Frequencies of gene rearrangements in HLH associated lymphomas were contrasted to non-HLH associated lymphomas within the Mitelman database. Data was analyzed using Microsoft Excel and GraphPad Prism. All p-values are two- sided and results ≤0.05 were considered significant.
Results:
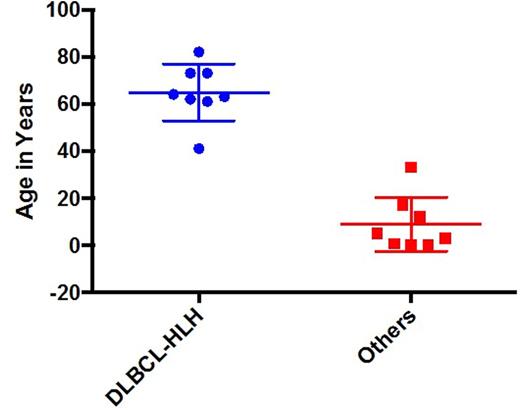
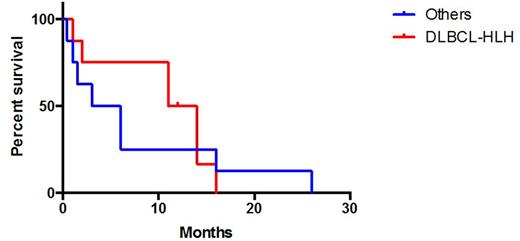
16 pts with HLH associated B-cell lymphomas were identified. 8 pts had DLBCL associated HLH, 5 had EBV associated B-cell lymphomas and 3 had B-cell lymphomas NOS. The 8 pts without DLBCL were considered as a single group for further analysis. Pts with DLBCL-HLH were significantly older (mean 64.9 years, range 41-82) than the others (8.9, 0.3-33, t-test <0.0001) (Figure 1). 75% (6/8) of DLBCL-HLH pts were male vs 63% (5/8) of others. Median LDH, median ferritin, and median IL-2R were 1,117 (U/L), 1,073 (ng/mL), and 13,323 (pg/mL) respectively in the DLBCL-HLH pts and these were not reported in the others. 88% (7/8) pts with DLBCL-HLH received CHOP while 100% (8/8) of the others received etoposide and corticosteroids with or without other agents. DLBCL-HLH were more likely to harbor unbalanced rearrangements (75% v 13%, RR=3.9, 95%CI 1.1 - 13.6, p=0.04) and rearrangements in immune related loci (9p24 - PDL1/2 (2), 19q13 - IFN lambda 1,2,3 (2), and 12p11 - DDX11 (1)) versus none in the others (63% v 0%, RR=3.7, 95%CI 1.4 - 9.6, p=0.03). One pt each with DLBCL-HLH harbored rearrangements of MYC (1/8) and BCL2 (1/8) while none of the others had rearrangements in MYC or BCL2. No patient in either group had a rearrangement of BCL6. Median overall survival was 12.5m in DLBCL-HLH versus 4.5m in the others (log rank p=0.23) (Figure 2).
Compared to non-HLH associated cases of DLBCL within Mitelman the incidence of rearrangements and additions in the immune related loci 9p24 (25% (2/8) v 3% (37/1413) (p=0.02)), 19q13 (25% (2/8) v 4% (61/1413) (p<0.05)) and 12p11 (13% (1/8) v <1% (6/1413) (p=0.04)) were significantly higher in DLBCL-HLH.
Conclusion:
DLBCL-HLH is a distinct entity with dismal outcomes with standard chemotherapy and frequent rearrangements of immune related genes. Novel treatment strategies are needed and may include immune modulatory agents such as PD-1 inhibitors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal