Abstract
Background Over 55% of all NHL is diagnosed after age 65y. Declining death rates have resulted in a growing population of older NHL survivors. However the long-term morbidity and mortality in this population remains unknown. This study addresses this gap by evaluating post-cancer late morbidity and mortality experienced by 2y NHL survivors diagnosed at age ≥65, using data from SEER linked with Medicare claims, and an age, sex and race frequency-matched comparison group derived from and representing 5% of the Medicare non-cancer population.
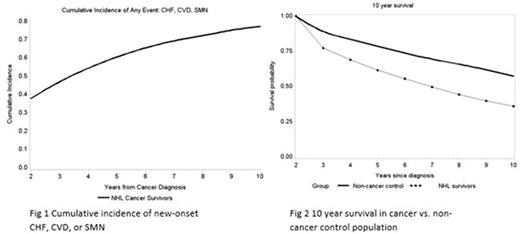
Methods Individuals ≥67y of age (to allow for identifying pre-cancer conditions) with incident NHL diagnosed between 1/1/2000 and 12/31/2008 and surviving at least 2y (n=10,958) were included in this analysis. Survivors were diagnosed as aggressive NHL (diffuse large B cell, Mantle cell, Burkitt's: n=7,004) or indolent NHL (follicular, marginal zone, chronic lymphocytic and small cell lymphocytic leukemia: n=3,954). New-onset morbidity: Competing risk cumulative incidence functions were used to assess the development of new-onset morbidity (congestive heart failure [CHF], cardiovascular disease [CVD: stroke/ myocardial infarction], and subsequent malignant neoplasms [SMNs]). Cox regression models evaluated predictors associated with new-onset morbidity. Predictors included lymphoma type (aggressive vs. indolent), age at NHL diagnosis, stage, sex, SES, race/ethnicity, radiation site, chemotherapy (none, rituximab only, anthracycline based chemotherapy (ABC), non-ABC chemotherapy), and pre-cancer comorbidity (Charlson Comorbidity Index + hypertension + depression). Late mortality: Kaplan-Meier methods were used to evaluate all-cause late mortality and cumulative incidence to evaluate cause-specific mortality.
Results: The median age at NHL diagnosis was 76y (range: 67-103) with a median survival of 7y (2-14y); 55% were male, 90% were Non-Hispanic White and 39% resided in an area where >10% of the population lived below poverty level; 64% were diagnosed with aggressive NHL; 39% received ABC therapy and 20% received radiation (n=2,219). New-onset morbidity: The 10y cumulative incidence of new-onset morbidity was greater among survivors compared to the comparison group: CVD (57.4% vs. 53.8%, p=<0.001), CHF (56.0% vs. 43.1%, p<0.001). Controlling for pre-cancer comorbidities, cancer survivors were at 1.7-fold increased risk of developing new-onset CHF (p<0.001), 1.16-fold increased risk for CVD (p<0.001) compared to non-cancer population. Multivariable analysis among survivors revealed that those who received ABC were at 1.21-fold increased risk of developing CHF (p<0.001) and those treated with non-ABC were at a 1.13-fold increased risk (p=0.01). Survivors who received radiation to the chest/axilla were 1.14-fold more likely to have a CVD compared to those without radiation (p=0.03). The 10y cumulative incidence of SMNs among NHL survivors was 21.6%. The most common SMNs were lung cancer (13.1% of all SMNs) and prostate cancer (11.2%). Survivors who received any radiation were at 1.37-fold (p<0.001) increased hazard of developing an SMN compared to those without radiation. Importantly, the 10y cumulative incidence of one or more of the new-onset morbidities (CHF, CHD or SMNs) was 77.3% among the NHL (Fig 1). Late mortality: Conditional on surviving the first 2y, the overall survival was 61.2% at 5y from diagnosis and 35.8% at 10y, significantly lower than matched controls at equivalent time points (78.7%, 57.5%; p<0.0001) (Fig 2). Controlling for pre-cancer comorbidities, individuals with aggressive NHL were at 2.0-fold (p<0.001) increased risk and those with indolent NHL were at 1.9-fold (p<0.001) increased risk of late death compared with the matched control population. Among survivors, the 10y cumulative incidence of lymphoma-related death was 38.1%, CVD-related death (19.9%) and SMN-related deaths (13.6%).
Conclusion The incidence of new-onset morbidity exceeds 75% at 10yfrom diagnosis ofNHL in the elderly. Further, 2y NHL survivors are at a 2-fold increased risk for late mortality when compared with a non-cancer population. These findings provide evidence for the need for close long-term risk-based medical follow-up of elderly with NHL.
Mehta:Pharmacyclics: Research Funding; Medimmune: Research Funding; Bristol Myers Squibb: Research Funding; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees; Roche Genentech: Research Funding; Incyte: Research Funding; Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal