Abstract
Idiopathic cytopenia of undetermined significance (ICUS) includes a highly heterogeneous population with unknown natural history; however, some patients develop clonal mutations of 1/2/3 cell-lineages and subsequently bona fide MDS/AML. A situation of blood-cytopenia and marrow-dysplasia often indicates MDS, which represent heterogeneous pre-malignant hematopoiesis with risk of AML. Cytogenetics has detected chromosomal alterations in MDS, including del(5q), -7/del(7q), del(9q), -13/del(13q), del(11q)/t(11q), del(12p)/t(12p), -17/del(17p)/i(17q), +19/t(19) and idic(Xq13) even in absence of morphological dysplasia. MDS-specific somatic mutations/chromosomal aberrations have been reported in >30% cytopenic patients. Present knowledge on mutational landscapes in mRNA-splicing, DNA-methylation and many other pathways in elderly individuals with hematopoietic and/or non-hematopoietic disease has redefined the clinical impact of clonal hematopoiesis of indeterminate potential (CHIP) and pathobiology of MDS/AML. Considering the power of conventional cytogenetics entrusted by recent WHO-2016 classification for risk-scoring, and also the resource setting available in developing countries, we performed cytogenetics for prognostication of on 1693 Indian cytopenic cases suspected with MDS.
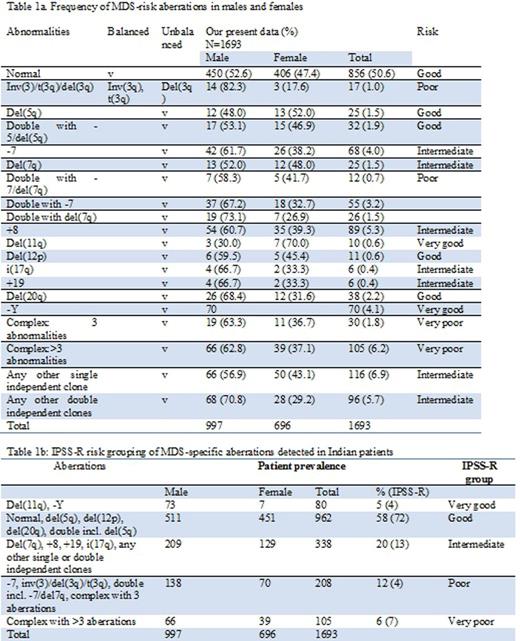
Conventional cytogenetics has described the novelty of comprehensive chromosomal picture as single and double independent clones and monosmal (MK)/complex karyotypes (CK) in explicit combinations indicating co-occurrence elderly presented with uni-/bi-/pancytopenia in peripheral blood. Unstimulated culture of bone marrow cells was carried out following the standard protocol for G-banding cytogenetics. Complete 20-25 metaphases were analyzed with karyotypic classification of ~10 metaphases as per ISCN using IKAROS software (MetaSystems, Germany). The frequency of del(3q/5q/7q/11q/12p/20q), monosomy 5/7, trisomy 8/19/21, i(17q), -Y, and translocations have been categorized as single and double independent clone and in co-occurrence of MK and CK for IPSS-R risk-scoring. The classification of single (other than del(5q/7q), -(7/-Y) and +(8/21)) and double (two separate clones with different aberrations) independent clones, CK with ≥3 aberrations include any 3 of these or others have been followed. The drawback was lack of WHO/FAB classification of the patients and monitoring progression and treatment outcome.
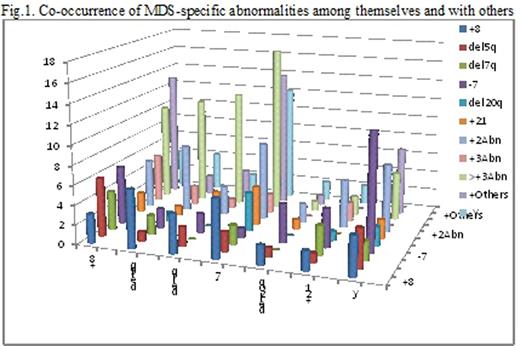
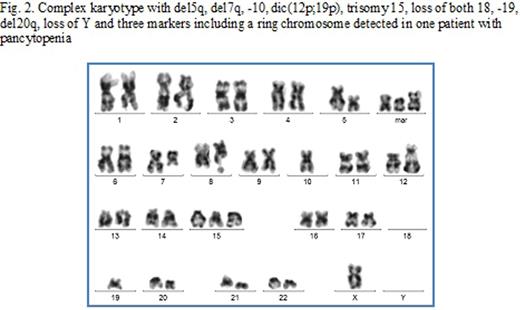
Among the specific rearrangements, CK with ≥3 aberrations (8%), other single (7%) and double (5.7%) independent clones, +8 (5.3%), -7 (4%) and - Y (4.1%) were highly prevalent (Table 1a). The combined frequencies of single and double independent clones (12.6%) were higher than CK with ≥3 aberrations (8%), in which CK with >3 aberrations were frequently noted. MK with chromosome 5 (1.8%) was lower than 7 (12.2%). Five-tier IPSS-R risk grouping revealed the patient-prevalence with del(11q) and -Y is in good correlation (Table 1b); however, the incidence was significantly higher for 'intermediate' and 'poor' risk-groups and lower for 'good' category, which is mostly influenced by variable frequencies of del(5)/-7/+8 in Indian patients. Co-occurrence of del7q and del20q was highly infrequent (Fig.1). Prognostic-signatures and pair-wise comparison of single exclusive and in combination were in concordance with literature, and are significant for understanding patho-biology and disease-spectrum in this population of different geographical location. Non-MDS 'cytogenetic-CHIP' was evident in 12% patients as single and double independent clones, for which MDS-diagnosis remains unfulfilled. One patient showed at least 9 aberrations in all of 25 cells screened (Fig.2).
This study recommends cytogenetic screening for cytopenic cases with ambiguous presentation and morphology. There could be significant delay in consulting a hematologist, especially for the villagers living below the border of sustainable economic condition, and therefore, opportunistic interaction of cooperating mutations and clonal expansions could be present at higher scale at pre-therapeutic stage. Cytogenetic risk-scoring of ICUS patients may be of tremendous help in absence of advanced technological resource setting.
References
1 Belli et al Am J Hematol 2011 86:540
2 Ganguly&Kadam Mutat Res 2016 769:47
3 Kwok et al Blood 2015 126:2355
4 Steensma et al Blood 2015 126:9
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal