Abstract
Background: Clonal hematopoiesis in elderly patients without evidence for overt hematologic malignancy (i.e., myelodysplastic syndrome [MDS] and acute leukemia) is associated with elevated Red-Cell-Distribution-Width (RDW). A correlation between high RDW, detectable myeloid mutation and cardiovascular dysfunction (CVD) suggests that inflammation is central to development of clonal hemopoieisis and cardiovascular disease. Anemia, especially linked with elevated RDW is frequently observed in patients with CVD (congestive heart failure [CHF], coronary artery disease [CAD]). Animal models suggest that increased TNFα and activated lymphocytes lead to stem/progenitor hemopoeitic failure during CHF exacerbation. Despite a well-known effect of comorbidities on MDS outcome, the impact of CVD on erythropoiesis prior to development of overt MDS remains uncharacterized. We reasoned that inflammation originating from CVD could not only direct progressive chronic RDW change prior MDS diagnosis but also that those RDW modifications could differ from subgroup of pts without CVD.
Methods: RDW data leading up to the diagnosis of MDS was collected retrospectively from79 patients stratified according to MDS-comorbidity index. Patients were analyzed to determine if comorbidity was present at the time of first detectable RDW abnormality. Datapoints suggesting GI bleed, hemolytic anemia, thalassemia trait, iron and B12 deficiencies were excluded. Timescales were designed to record, in each pt, first detectable RDW followed by all available time- aligned datapoints until the time of diagnosis. The presence of left ventricular dysfunction, CAD and either CHF or CAD associated with atrial fibrillation were considered CVD. Pt with non-CVD comorbid condition (CC) or without comorbidity were assigned to the non-CVD subgroup. A linear regression model was used to evaluate correlation between RDW modifications and time-progression prior to MDS diagnosis. R-squared calculations allowed investigation for strength of association between observed RDW means and fitted regression line among pts with and without CVD.
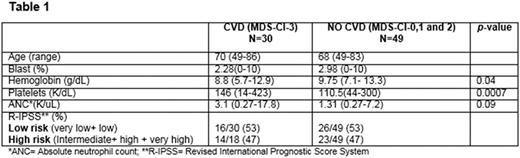
Results: Disease characteristics among pts with and without CVD are depicted in table 1. Age, blast count, and R-IPSS subgroups were balanced in both groups. Hemoglobin for pts with and without CVD was 8.8 g/dL vs 9.75 g/dL, respectively (p=0.04). For pt with evidence of CVD, higher platelet count was observed (146 K/uL and 110.5 K/uL, respectively, p= 0.0007). Linear regression revealed that RDW modifications co-evolve overtime in pts with and without CVD (p=0.0001 for both groups) Fig 1. However, a stronger association between time evolution and RDW modifications was observed in pt with CVD vs those without CVD (R2 =.66% vs 0.61%, respectively)
Conclusion: Progressive RDW modifications occur months to years before MDS diagnosis. Sequential time-dependent RDW modifications in pts with CC suggest a link between defects in erythropoiesis and comorbidity prior MDS diagnosis. Our results support the view that evolutionary RDW modifications underpin the capacity of hemopoieitic stem cells to adapt to adverse organ function, especially in pt diagnosed with CVD experiencing anemia. Our study represents a conceptual framework for investigation of the initiation of clonal hematopoiesis in an aging population with CVD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal