Abstract
Background: Febrile neutropenia is associated with significant morbidity, mortality, healthcare resource utilization and associated cost. However, data regarding the relationship of specific cancers with admission for febrile neutropenia and their outcomes is lacking.
Methods: Using the ICD-9 codes 288.00 and 288.04, we identified all adult admissions with primary diagnosis of febrile neutropenia during the interval of 2006-2013 from the Nationwide Inpatient Sample (NIS). Hospitalization information regarding mortality rates, length of stay and total charges was extracted for each year. Total cost was adjusted for inflation using data from the U.S. Bureau of Labor Statistics. Differences in these variables in teaching and nonteaching institutions were evaluated. ICD-9 codes for esophageal, colon, rectal, liver, pancreatic, bladder, prostate, cervical, renal, thyroid, lung, and melanoma skin cancers were selected and the percentage of admissions attributed to each malignancy was determined.
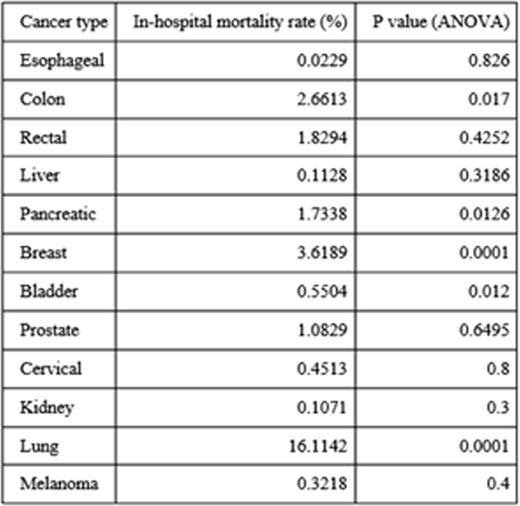
Results: We identified 48,253 admissions (weighted N = 233,116) with a primary diagnosis of febrile neutropenia from 2006-2013. Most of these admissions occurred at teaching institutions (n=28,902, weighted n=139,574). In-hospital mortality rates for febrile neutropenia had a downward trend over the time period of 2006-2013 although the difference was not statistically significant (p=.082). Specifically, the in-hospital mortality rate was 2.73% in 2006 and 1.35% in 2013. Mean length of stay (days) has decreased from 5.67 (±.16) in 2006 to 5.32 (±0.06) in 2013 (p=.0001) while total charges have increased from $29,113 (±1089) in 2006 to $41,713 (±726) in 2013 (p=.0001). This is greater than the expected inflationary change from $29,133 to $33,641 over the same time period. Mean length of stay (days) was found to be higher at teaching (5.89±.03) than at non-teaching (5.25±.04) hospitals (p=.0001). Similarly, mean total charges were higher in teaching ($41,577±364) than in non-teaching ($34,176±345) institutions (p=.0001). When comparing teaching vs. non-teaching institutions, in-hospital mortality was not found to have a statistically significant difference (p=.2688). Of the 13 malignancies queried, lung cancer (11.06%) and breast cancer (8.40%) accounted for more admissions for febrile neutropenia than the other malignancies selected. Breast cancer (3.62%, p=.0001) and lung cancer (16.11%, p=.0001) were also associated with much higher in-hospital mortality rates compared with the other malignancies selected.
Conclusions: Breast and lung cancer account for a significant number of admissions for febrile neutropenia, which is consistent with their national prevalence. Of particular note,breast and lung cancer patients who were admitted for febrile neutropenia had a higher risk of mortality. In lung cancer, the frequently associated smoking-related comorbidities may be contributing to this finding. While in breast cancer, patients with advanced disease have an increase in cumulative lifetime dose of chemotherapy due to prolonged survival and this may result in a weakened bone marrow, a more susceptible patient, and consequently an increase in febrile neutropenia and mortality rates. Thus, given the greater mortality rate and significant number of patients affected, patients with these two malignancies should receive special attention to ensure they receive prophylaxis with granulocyte stimulating agents and/or antibiotics after treatment with cytotoxic chemotherapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal