Abstract
Background: The optimal follow-up of MGUS patients, including frequency of visits and type of tests to order, is unknown because there are no evidence-based data available for guidance. Nevertheless, there are currently 4 clinical practice guidelines that are based on expert-consensus: UK-Nordic (2009), International Myeloma Working Group (IMWG; 2010), International Expert Consensus (IEC; 2010) and European Myeloma Network (EMN; 2014). Most guidelines recommend annual follow-up with laboratory tests until life expectancy becomes limited. How MGUS patients are followed in the US and whether clinical practice guidelines are being followed remain largely unknown.
Methods: We conducted a retrospective analysis of adult (age >18 years) patients from 2006-2012 using theOptum Labs Data Warehouse,a large database including administrative claims information on >150 million privately insured and Medicare Advantage enrollees throughout the US. We identified patients with an incident diagnosis of MGUS (ICD9: 273.1) who had enrollment periods of>1 year pre- and>2 years post-diagnosis in order to exclude patients with a prior history or subsequent diagnosis of lymphoplasmacytic malignancy. We determined the overall outpatient follow-up practice patterns (visits or tests performed for MGUS), their variations over time and by geo-demographic subgroups, and concordance with current clinical practice guidelines
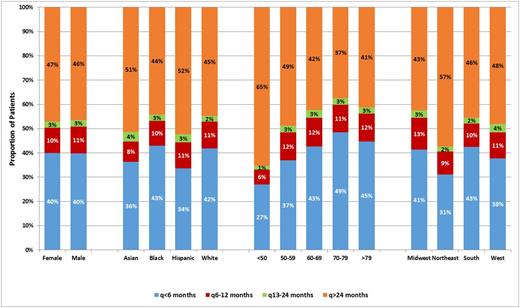
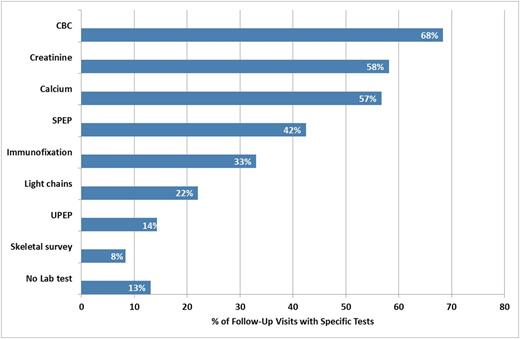
Results: There were 10,349 MGUS patients who met the study criteria. The mean interval per MGUS follow-up visit was 13.1 months. The distribution of patients by mean interval between visits was: q<6 months (39.9%), q6-12 months (10.7%), q13-24 months (2.6%) and q>24 months (46.8%). There was a significant trend towards a higher proportion of patients being followed q<6 over time from 36.2% in 2006 to 43.7% in 2013 (P=0.01). Patients ≥70 years were more likely followed q<6 months, while those from the Northeast or ≤50 years were more likely followed q>24 months compared to their counterparts (P<0.01). Over half of patients≥80 years were being followed either q<6 (44.7%) or q6-12 (11.6%) months (Figure 1). Only about half of the patients diagnosed in 2013 were concordant with any of the available guidelines regardless of whether the guidelines were more aggressive (UK-Nordic/IEC) or more conservative (IMWG/EMN) in their follow-up recommendations (54.6% and 56.5%, respectively). The tests ordered during follow-up are shown in Figure 2. The most common tests were complete blood count, calcium, and creatinine as they were ordered in over half of the follow-up visits (56.5% to 68.4%). In 11.6% of the follow-up, a face-to-face visit was not associated with any ancillary test, while in 31.5%, the follow-up was comprised of ancillary tests only without a face-to-face visit. The test combination of complete blood count, calcium, creatinine, and serum protein electrophoresis with or without free light chain was ordered in 25.0% of the visits.
Conclusions: In the US, the MGUS follow-up practice patterns varied demographically and geographically. Only half of the patients were followed according to current guideline recommendations. A large proportion of patients with limited life expectancy continued to undergo close follow-ups.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal