Abstract
Introduction:
DLBCL is a heterogeneous disease with increasingly complex treatment selection. Prior studies demonstrated improved outcomes of hematologic malignancies managed in academic centers and based on socioeconomic factors. We aimed to compare OS of patients with DLBCL based on the type of treatment facility and other factors.
Methods:
This retrospective study utilized the National Cancer Data Base (NCDB) to identify patients with DLBCL diagnosed between 1998 and 2012. Health care facilities were categorized as either academic (academic/research program) or non-academic (comprehensive community cancer program, community cancer program, and other programs). Patients with complete data for sex, age, race, education, income, distance traveled for health care, hospital type, facility location, urban/rural, insurance, Charlson co-morbidity score, chemotherapy use, time from diagnosis to treatment initiation, use of hematopoietic stem cell transplant, last contact, and vital status were included. OS of patients who received first course treatment at academic centers, was compared to those treated at non-academic centers. Kaplan Meier curves for OS were compared using log-rank test. Multivariate Cox proportional hazard model was performed to identify determinants of OS.
Results:
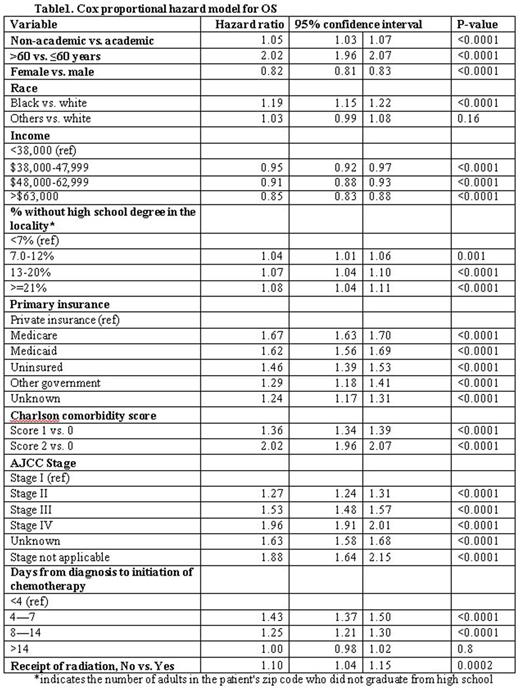
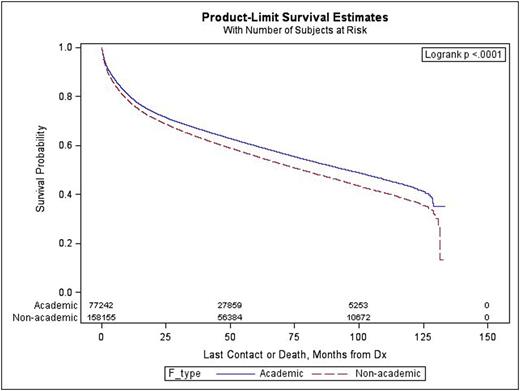
Of 264,697 patients with DLBCL, 33% were treated at academic centers. Patients treated at academic centers differed from non-academic centers in mean age (65 vs. 68 years; p <0.0001), gender (45 vs. 47% females, p <0.0001), race (85 vs. 91% whites, p <0.001), income (38 vs. 31% with annual income >$63,000, p <0.001), education (17 vs. 15% residing in locality with ≥21% population without high school graduates, p <0.001), and insurance status (40 vs. 35% with private insurance, p <0.001), Charlson comorbidity score (79 vs. 76% with score 0, p <0.001) and AJCC stage (40 vs. 33% stage IV, p <0.001). Because of missing data, only 167,458 patients were used for OS analysis. Receipt of first course treatment at academic versus non-academic centers was associated with a higher median OS (95 months vs. 78 months, p<0.0001) (Figure 1). After adjusting for other co-variates, treatment at non-academic centers was associated with an increased risk of death (hazard ratio 1.05, 95% confidence interval 1.03-1.07). Other factors associated with improved OS include younger age, female sex, white race, private insurance, higher income and educational status, lower stage, lower comorbidity score, early initiation of chemotherapy, and use of radiation therapy (Table 1).
Conclusion:
Our study demonstrated differences in the characteristics of patients with DLBCL based on the facility type. Academic centers were more likely to treat patients who were younger, females, of ethnic minorities, with less education, higher income levels, private insurance, less comorbidities and higher stage disease. The receipt of frontline therapy at academic centers was associated with increased OS in patients with DLBCL. Some of the possible reasons for this difference may include provider experience, increased access to resources and clinical trials. Our study also demonstrated cancer health disparities based on other socioeconomic factors such as gender, race, income and insurance status. Further investigations into the factors contributing to such disparities should be a research priority to help standardize care and improve outcomes.
Armitage:Conatus - IDMC: Consultancy; Roche: Consultancy; Spectrum Pharmaceuticals: Consultancy; GlaxoSmithKline IDMC: Consultancy; ZiopharmOncology: Consultancy; Tesaro bio Inc: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal