Abstract
Background: The natural histories of aggressive and indolent NHL vary in terms of the timing and pattern of disease progression. However, little is known about the impact of progression of disease (PD) on costs, and in particular how this differs between aggressive and indolent subtypes of NHL. This study examined patterns of care and outcomes for patients with aggressive and indolent NHL, and the impact of PD on health care costs.
Methods: To identify cases of NHL, this retrospective studyused medical and pharmacy claims from a large national US health plan to identify commercially insured and Medicare Advantage (MA) patients age ≥18 years from 1/2007 - 8/2014 with ≥2 medical claims for NHL based on ICD-9-CM diagnosis codes. Patients were divided into cohorts of aggressive (AGG) NHL and indolent (IND) and based on diagnosis codes. Patients were required to have ≥1 claim for systemic anti-cancer therapy, with the index date being defined as the first observed claim for such therapy. Continuous enrollment in the health plan for 6 months prior to (baseline period), and ≥6 months after, the index date (variable follow-up period) was required; patients with <6 months of follow-up due to death were included. An algorithm to identify line of therapy (LOT) periods was implemented. PD was defined as: start of a second LOT, receipt of hospice care (based on procedure or revenue codes) or death (based on Social Security Administration death data). Health care costs were calculated over 6-month periods of follow-up (6, 12, 18, 24 months), with costs calculated for pharmacy, inpatient hospital, ambulatory, and other sites of service.
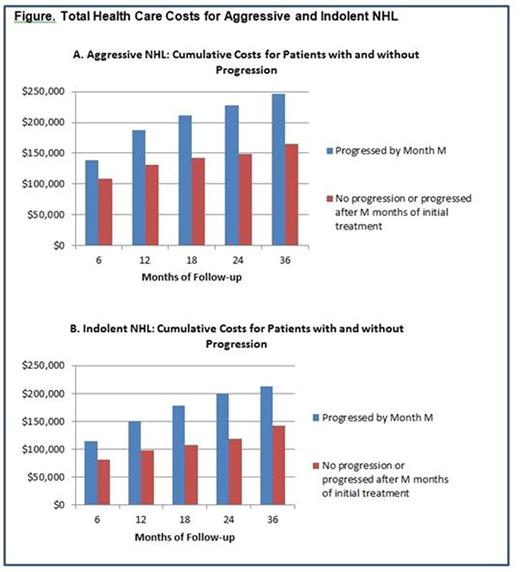
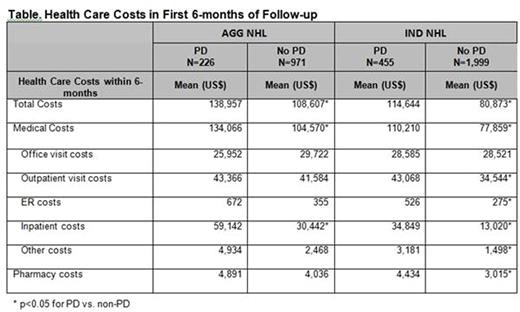
Results: A total of 1,197 AGG and 2,454 IND patients met study criteria. Progression was experienced by 40.6% of AGG and 49.4% of IND patients respectively during the entire study period; 6-month progression was 18.9% (AGG) and 18.5% (IND). Compared to patients without PD during the study period, patients who progressed had higher average costs over each time period: in the first 6-months, costs were $138,957 PD vs. $108,607 for non-PD among AGG, and $114,644 PD vs. $80,873 for non-PD among IND (Figure, Table). Similarly, total costs for PD were higher than non-PD over 12, 18, and 24 months (Figure). Costs by site of service were higher for PD patients compared to non-PD patients among both the AGG and IND groups, particularly for inpatients costs; the table shows costs by site of service for the first 6 months, and results were similar over 12, 18, and 24 months. A higher proportion of AGG patients died compared with IND patients. Approximately one third of patients who died used hospice services among AGG and IND, and of these, 90.1% of AGG and 91.3% of IND used 3 or more days of hospice care.
Conclusion: Among both aggressive and indolent NHL populations, costs were higher for patients with progressive versus without progressive disease, and increased over longer follow-up time. Patients with aggressive NHL had higher costs compared with patients with indolent NHL for both progressive and non-progressive disease. This study is the first to quantify systematically the cost of progression in NHL, both indolent and aggressive, and can inform efforts to improve value-based care, taking into account costs not just of therapy, but of subsequent progression.
Engel-Nitz:Optum: Employment, Other: UnitedHealth Group stock. Dacosta Byfield:UnitedHealth Group: Equity Ownership; Optum: Employment. Bancroft:Optum: Employment, Other: UnitedHealth Group stock. Amy:Optum: Employment, Other: UnitedHealth Group stock. Reyes:Genentech: Employment; Roche: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal