Abstract
Background: Thrombocytopenia (TCP) is commonly seen in chronic Hepatitis C (HCV). Ledipasvir-sofosbuvir (LDV/SOF) is a novel, fixed-dose anti-HCV combination that has shown high sustained virologic response (SVR) rates. However, since much remains to be learned about the natural history of TCP following LDV/SOF treatment, we set out to examine platelet (PLT) counts in thrombocytopenic patients with chronic HCV before, during, and after treatment with LDV/SOF.
Methods: This is an IRB-approved, retrospective study of patients diagnosed with chronic HCV who received LDV/SOF between November 2014 and April 2016 at the Washington DC Veterans Affairs Medical Center. Patients who had PLT counts less than or equal to 150 x 109/L for at least 6 months prior to treatment andcompleted therapy with LDV/SOF were included. Patients diagnosed with heparin-induced TCP; disseminated intravascular coagulation; medication-induced TCP; sepsis; as well as those who received PLT transfusion or thrombopoietic agents were excluded. PLT counts were collected at baseline (within 6 months prior to the start of therapy), during treatment, and throughout the follow-up period until the last follow-up, initiation of a new HCV medication, liver transplant, or death. Patients were categorized into 3 groups: mild TCP (100-150 x 109/L), moderate (50-99 x 109/L), and severe (<50 x 109/L). Paired t-test was used to compare pre-treatment, on-treatment (week 4), and the last measured PLT counts. Multivariate regression analysis was used to determine the baseline variables associated with improvement in PLT counts. All registered PLT counts from the start of therapy were included in repeated measurement analyses to assess the evolution of PLTs over time.
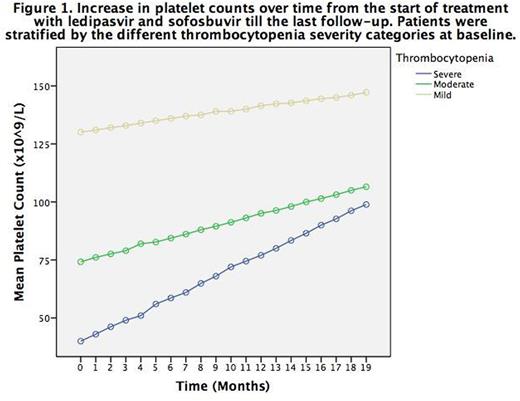
Results: Inclusion criteria were met in 244 patients (median age 64, 98% male, 88.9% African American). HCV genotypes were 1a (77.4%) and 1b (22.6%). The median follow-up from treatment start was 13 months. Treatment duration was 8 weeks (13.9%), 12 weeks (69.7%), or 24 weeks (16.4%), all at the fixed dose of LDV 90 mg and SOF 400 mg once daily. SVR at 12 weeks (SVR12) was attained in 159 patients (65.2%) while 67 patients (27.5%) had a documented undetectable viral load earlier than 12 weeks from treatment completion with no further testing. Eight patients (3.3%) failed treatment and 10 (4.1%) were lost-to-follow-up. The mean pre-treatment PLT count was 114 x 109/L (22-150). The on-treatment and last measured PLT counts were significantly higher than the baseline PLT count (129 x 109/L, p<0.001 and 144 x 109/L, p<0.001 respectively). The increase from the on-treatment to the last measured PLT count was also statistically significant (p=0.008). The last measured PLT counts were on average 32.8 ± 66.7% higher than the baseline and 31.6% of patients had normal last measured PLT counts. The increase in PLT count was observed for all three TCP groups: mild (73.4%): from 129 x 109/L at baseline to 149 x 109/L during treatment (p<0.001) to 160 x 109/L after (p=0.045); moderate (24.2%): from 75 x 109/L before to 89 x 109/L during (p=0.004) to 112 x 109/L after (p=0.027); severe (2.5%): from 38 x 109/L before to 64 x 109/L during (p=0.003) to 97 x 109/L after (p=0.234). Multivariate regression analysis was performed including the following variables: age; gender; HCV genotype; baseline PLT count, albumin, bilirubin, and AST/ALT; history of severe alcohol abuse; HIV coinfection; Hepatitis B coinfection; presence of splenomegaly; presence of cirrhosis; treatment duration and reaching SVR12. It showed that reaching SVR12 is associated with a faster increase in PLT count (p=0.022). Repeated measurement analyses showed a gradual and linear increase in PLT counts from the start of therapy for the entire cohort (p<0.001) as well as in every TCP group: mild (p<0.001), moderate (p=0.001) and severe (p=0.015).
Conclusion: LDV/SOF is associated with an increase in PLT counts in chronic HCV patients with TCP. This desired effect becomes apparent even before the conclusion of therapy. It is thus tempting to correlate the increase in PLT count with LDV/SOF-associated quick eradication of HCV soon after treatment initiation. Whether that is due to elimination of HCV-associated bone marrow suppression and autoimmune TCP or other not yet known mechanisms, these results are tantalizing but would require longer follow-up. Larger prospective studies are needed to ascertain these results and uncover potential mechanisms.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal