Abstract
Background: In chronic myeloid leukemia (CML) the combination treatment of tyrosine kinase inhibitors (TKIs) with interferon-α (IFN-α) has proved to be effective and well-tolerated. IFN-α has long-term immunomodulatory effects, and when combined to TKI therapy, it may increase the success rates for treatment free remission. In our recent clinical trial NordCML007, a low-dose pegylated IFN-α was combined with dasatinib therapy. As dasatinib is also known to have immunostimulatory effects (activation of T and NK cells and downregulation of regulatory T cells), we aimed to monitor the immune effects of dasatinib and IFN-α combination treatment.
Methods: 40 newly diagnosed CML patients participated in the NordCML007 clinical trial (NCT01725204). Patients were treated with 100 mg dasatinib QD and after 3 months IFN-α treatment was added (first 3 months 15 μg/week, then 25 μg/week of pegylated IFN-α). After 12 months of combination treatment, patients resumed to dasatinib monotherapy. In this immunological substudy, peripheral blood samples were collected at the diagnosis, 3, 12, and 24 months after the start of therapy. T- and NK-cells were phenotyped with multicolor flow cytometry, and their function (degranulation and cytokine secretion) was studied. In addition, a multiplexed cytokine and growth factor panel was performed (Proseek Multiplex Inflammation I96×96, Olink).
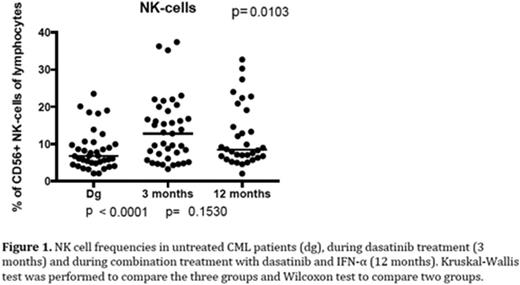
Results: Dasatinib monotherapy led to an increase of NK-cell frequencies when compared to pre-treatment values (median diagnosis 6.8% vs. 3 months 12.8%, p<0.0001, Figure 1). In contrast, the proportion of B cells decreased (6.0% vs. 3.8%, p=0.001). Also moderate effects on the T cell subsets were observed (CD4+ 53% vs. 58%, p=0.02; CD8+ 47% vs. 43%, p=0.03).
The more detailed immunophenotyping showed that at 3 months NK cells were more mature when compared to pre-treatment values. This could be observed as the increased proportion of CD16+ (86% vs. 77%, p=0.008) and CD57+ (79% vs. 67%, p=0.0001) NK cells. Correspondingly, the frequencies of CD56bright (median 3 months 3.9% vs. dg 6.1%, p<0.0001) and CD27+ (median 3 months 31.2% vs. dg 58.2%, p=0.004) NK cells decreased. The degranulation responses of NK cells when stimulated with K562 cells were also decreased (median 27.4% vs. 35.5% of CD56+ NK cells, p=0.02).
Similar effects of dasatinib treatment were also observed within the T cell population, and at 3 months patients had more CD8+ terminally differentiated effector memory CD45RA+ (Temra) cells (22% vs. 32%, p=0.03). Correspondingly, both CD8+ and CD4+ effector memory (EM) populations decreased (CD8+ EM 34% vs. 24%, p=0.007; CD4+ EM 21 % vs. 14 %, p=0.0003). As observed with the NK cells, the degranulation and Th1 type cytokine secretion of T cells decreased during dasatinib treatment (CD107a/b+ 19.4% vs. 18.4% of CD8+ T cells, p=0.02; CD107a/b+ 12.7% vs. 8.8% of CD4+ T cells, p=0.005). Interestingly, 3 out of 4 patients who suffered from pleural effusion (PE) had exceptionally high CD57+CD8+ T cell frequencies (>70% of CD8+ T cells, median 38% in all patients) at diagnosis and during the treatment.
The combination of IFN-α did not significantly affect the number of NK cells. Interestingly however, the addition of IFN-α treatment seemed to have an opposite effect on the NK cell phenotype than dasatinib treatment. The proportion of CD56bright NK cells increased (median 3 months 3.9% vs. 12 months 5.2%, p=0.03), and a decreasing trend was observed among CD16+ and CD57+ NK cells at 12 months. Similarly, the T cell surface markers shifted towards more immature phenotype (CD4+ EM 14% vs. 19%, p=0.002; CD4+ CM 36% vs. 28%, p=0.002; CD8+ Temra 32% vs. 17%, p=0.003) and the degranulation of CD4+ T cells and NK cells returned to the diagnosis level.
The initiation of dasatinib treatment was associated with a decrease in several plasma protein concentrations (IL-18, IL-8, CXCL5, MCP-2, MCP-3, VEGF-A, CD244, LAP TGFβ1, TGFA, 4E-BP1, ADA, STAMPB, Casp8, OSM) and an increase in others (SCF, MCP-1). After IFN-α addition, the concentration of MCP-1 was further increased.
Conclusions: These results show that dasatinib and IFN-α modulate both innate and adaptive immune systems. Interestingly, where dasatinib seems to induce a more mature immunophenotype, IFN-α counteracts this by driving a shift towards a more immature phenotype. Comparative analysis of the changes in the immunophenotype and function with the clinical outcome of the patients is ongoing.
Stentoft:Ariad: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Bristol-Myers-Squibb: Research Funding. Richter:Pfizer: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Ariad: Honoraria, Research Funding. Höglund:Akinion Pharmaceuticals: Consultancy; Janssen-Cilag: Honoraria. Mustjoki:Ariad: Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal